Schedule at a Glance
Monday, October 2nd
Tuesday, October 3rd
| 6:30 a.m. – 8:00 a.m. | Breakfast and Presentation
Presented by
 |
| 8:15 a.m. – 9:15 a.m. | Keynote Speaker: Cy Wakeman |
| 9:15 a.m. – 10:45 a.m. | Exhibit Hall Open (Morning Motivational Meetup!) |
| 10:45 a.m. – 12:00 p.m. | Concurrent Breakout Sessions |
| 12:00 p.m. – 12:45 p.m. | OR Manager Awards Presentation and Luncheon |
| 12:45 p.m. – 2:00 p.m. | OR Manager Awards Dessert Reception in the Exhibit Hall |
| 1:00 p.m. – 2:00 p.m. | Poster Sessions |
| 2:00 p.m. – 3:15 p.m. | Concurrent Breakout Sessions |
| 3:15 p.m. – 4:30 p.m. | Exhibit Hall Open (Refresh, Relax, Recharge!) |
| 3:30 p.m. – 4:30 p.m. | Poster Sessions |
| 4:30 p.m. – 5:30 p.m. | Keynote: Dennis Snow |
| 7:00 p.m. – 10:00 p.m. | OR Manager’s Night Out
|
Wednesday, October 4th
| 6:00 a.m. – 7:00 a.m. | Morning Walk and Talk |
| 6:30 a.m. – 8:00 a.m. | Breakfast and General Session: Joe Tye Presented by  |
| 8:15 a.m. – 9:30 a.m. | Concurrent Breakout Sessions |
| 9:45 a.m. – 11:00 a.m. | Concurrent Breakout Sessions |
| 11:00 a.m. – 11:15 a.m. | Morning Break |
| 11:15 a.m. – 12:15 p.m. | Closing Keynote Speaker: Vicki Hess, MS, RN, CSP
Sponsored by
|
Keynote Speakers






The 2017 OR Manager Conference will feature four Keynote Speakers who will engage, inspire, and delight you with their experiences and lessons learned throughout their lifetimes.
And if that’s not enough, Keynote Speaker sessions at the OR Manager Conference also count for additional contact hours!
Meet the 2017 Keynote Speakers
Changing the Equation: The Future of Your OR and PACU in the Ever-Changing Healthcare Environment
 David C. Chin, MD, MBA
David C. Chin, MD, MBA
Distinguished Scholar
Johns Hopkins Bloomberg School of Public Health
Monday, October 2
2:45 p.m. – 4:00 p.m.
After this session you’ll be able to:
- Summarize the major Federal and State Policies driving value-based purchasing of health care.
- Discuss and interpret the key financial levers in the US healthcare system and their implications for academic medical centers and clinicians.
- Review the ever-changing healthcare landscape and what may be coming in the future.
- Understand your role in the future of healthcare.
Why this is important:
Healthcare costs have far outpaced predictions of the past, and with so many questions looming in 2017, it’s critical for perioperative leaders to be prepared to move their businesses forward. How did we get here? What will the next 5, 10, or 20 years look like for the healthcare landscape? How are we going to survive change? The new generation of healthcare workers will be responsible for transforming the industry into the value based system that it was always intended to be for the ultimate customer, the patient. Join us as Dr. Chin summarizes the major Federal and State Policies driving value-based purchasing of healthcare and shares his insights on the key financial levers in the current US healthcare system and their implications.
Sponsored by:
![]()
Ditch the Drama! Hard-Wiring New Mindsets and Accountability in Your Staff
 Cy Wakeman
Cy Wakeman
President & Founder, Reality-Based Leadership
Author, Reality-Based Leadership and The Reality-Based Rules of the Workplace
Tuesday, October 3
8:15 a.m. – 9:15 a.m.
After this session you’ll be able to:
- Apply strategies to reduce emotional waste resulting in improved quality metrics.
- Recognize behavior that enables teamwork and improved patient care.
- Implement leadership tools that hardwire accountability in your organization.
- Understand the cause(s) of drama in your workplace and how to change the mindsets of your staff.
Why this is important:
Old patterns of leadership thinking are no longer sufficient for today’s changing healthcare landscape. Cy Wakeman, President and Founder of Reality Based Leadership, notes that drama is at an all-time high – the average person working in the OR and PACU spends over two hours per day in drama. Therein lies the newest challenge for leaders – how do we motivate our teams to create amazing and safe patient experiences, great outcomes, all the while keeping staff engagement high and drama low? In this keynote, new tools for coaching and accountability will be revealed, empowering leaders to work through “learned helplessness,” rally their teams, and create the organizational alignment necessary to deliver extraordinary patient care.
The Magic of Customer Service: Training Your Staff for Excellence
 Dennis Snow
Dennis Snow
President, Snow Associates
Former Walt Disney World Company Executive
Tuesday, October 3
4:30 p.m. – 5:30 p.m.
After this session you’ll be able to:
- Discuss the four critical elements of service excellence.
- Develop tools for helping your team see the healthcare experience through the eyes of your customers.
- Understand customer expectations and approaches for exceeding those expectations.
- Determine mechanisms for involving your team in ongoing service improvement.
Why this is important:
Nurse leaders have numerous customers. In a single day, you interface with staff, physicians, other health care leaders, patients, families, and even in some cases, a board of directors. How can you view situations through their eyes, and use that perspective to create a culture of excellence in your organization? Providing world-class service in a healthcare setting is not simply a matter of smiling staff who say “please” and “thank you”. World-class service is an all-encompassing approach to making excellence business as usual, involving every member of the organization’s team. Developing a brand that identifies you and your team as providers of unparalleled customer care will give you the edge to be successful in the new normal health care environment. Join Dennis Snow, former Walt Disney World Company Executive, as he provides a “how-to” program for creating a service-driven culture.
Batten Down the Hatches: Engaging Your Team in Stormy Times
 Vicki Hess, MS, RN, CSP
Vicki Hess, MS, RN, CSP
Speaker, Trainer, and Consultant, Catalyst Consulting, LLC
Author, 6 Shortcuts to Employee Engagement: Lead & Succeed in a Do-More-with-Less World and SHIFT to Professional Paradise: 5 Steps to Less Stress, More Energy & Remarkable Results at Work
Wednesday, October 4
11:15 a.m. – 12:15 p.m.
After this session you’ll be able to:
- Understand the importance of transformational leadership as a means to improved engagement.
- Communicate with your staff in a way that everyone feels empowered.
- Create a system of shared responsibility for engagement.
- Deeply connect with your team so that you all feel re-energized and more motivated.
Why this is important:
Stormy times are ahead. Health care is transforming right before our eyes. As an OR leader, you are doing more with less, adapting faster, and managing uncertainty on the fly. How are your direct reports holding up? Are they adjusting quickly enough to keep up with the changing healthcare landscape? Transformational leaders work with their team to boost morale and increase engagement, as well as inspire a vision to guide change. In our closing keynote, fellow nurse, Vicki Hess, MS, RN, CSP, will equip you with the tools to successfully engage your team. You and your team will be ready to transform in the storm.
Speaker Gallery

R. Dan Allen
Founder and President
D. A. Surgical

Gail Avigne, MSN, BA, CNOR
Nurse Consultant
Press Ganey Associates, Inc.

Lisa A. Banks, MBA, BSN, RN, CPHQ
Quality Services Manager
Margaret Mary Health

Mark Barron
Principal Engineer
Sony Healthcare Solutions

J. Bryan Bennett
Professor
Northwestern University

Amy Bethel, RN, MPA, NE-BC
Clinical Education Specialist
UnityPoint Health Des Moines

Christopher Blackwell, PhD, ARNP, ANP-BC, AGACNP-BC, CNE, FAANP
Associate Professor & Coordinator, Adult-Gerontology Acute Care Nurse Practitioner Programs
College of Nursing, University of Central Florida

Jennifer Bonfili
RN Clinician
UPMC Presbyterian Hospital

Stephen Borstelmann, MD
Member Board of Directors
Columbia Club of the Palm Beaches, Inc.

Beth Bozzelli, MBA, RN, CNOR, CSSM
Assistant Vice President, Surgical Services
HCA Healthcare

Gabriel J. Bullaro, MBA
Chief Operating Officer
Ocala Health

Brenda Burk, MSN, BSN, RN, NEA-BC, CNOR
Director of Surgical Services
Lake Norman Regional Medical Center (CHS)

Elena G. Canacari, BSN, RN, CNOR
Associate Chief Nurse, Perioperative Services
Beth Israel Deaconess Medical Center
Phillip Chang, MD
Chief Medical Officer and Associate Professor, Trauma and General Surgery
University of Kentucky Healthcare

Desirée Chappell, MSNA, BSN, CRNA
Enhanced Recovery Expert, DLC Enterprises and Managing Editor
TopMedTalk

Dr. David C. Chin, MD, MBA
Distinguished Scholar
Johns Hopkins Bloomberg School of Public Health

Allan Joseph V. Cresencia, MSN, RN, CPN
Clinical Nurse II
Children's Hospital of Los Angeles

Bethany Daily, MHA, BA
Senior Administrative Director, Perioperative Services
Massachusetts General Hospital

Patricia M. DeFrehn, MBA, BSN, RN, NEA-BC
Baylor University Medical Center
Christina Dempsey, MSN, MBA, RN, CNOR, CENP, FAAN
SVP, Chief Nursing Officer
Press Ganey Associates, Inc.

Mary H. Diamond, MBA, RN, CNOR, PMP
Consultant

Tracy Diffenderfer, MSN, RN, CNOR
Administrative Director
Centennial Medical Center

Donna J. Doyle, DNP, RN, CNOR, NE-BC
Senior Advisor, Surgical Services
OhioHealth Grant Medical Center

Linda Easton, BS, RN
Infection Prevention Coordinator
Rochester Regional Health - United Memorial Medical Center

Mary Jane Edwards, MSHA, CNOR, FACHE
Deloitte Consulting

Roseles D. Escano, MPH
Specialist Master
Deloitte Consulting

Claire R. Everson, RN, CNOR, CCAP
Education Coordinator
SurgeryDirect, LLC

Sharon Finney, MJ, BS, CISSP
Director of Data Security
Adventist Health System

Lena Fogle, BSN, RN, CNOR
Director, Global Clinical Solutions
STERIS Corporation

Michelle C. Fortune, MBA, BSN, RN, CAPA, FACHE
Vice President Perioperative Services - Metro
Carolinas Healthcare System

Yvonne Gardner, MBA
Principal
Gardner & Associates

Jessica Geddings, BSN, RN, NE-BC, CSPDT
Director of Surgical Services
Citrus Memorial Hospital

Ann B. Geier, MS, RN, CNOR, CASC
Cheif Nursing Officer
SourceMedical

Bradley Getz, MD
Anesthesiologist
OhioHealth Grant Medical Center

Amy J. Goldberg, MD
Medical Director of Perioperative Services
Temple University Hospital

Charlotte Guglielmi, MA, BSN, RN, CNOR
Clinical Manager Perioperative Education
Beth Israel Deaconess Medical Center

Debbie Hall, MSN, RN, CNOR, NE-BC
Director of Surgical Services
Norton Audubon Hospital

Randall Heiser, MA, BA
President
Sullivan Healthcare Consulting

Vicki Hess, MS, RN, CSP
Author, 6 Shortcuts to Employee Engagement: Lead & Succeed in a Do-More-with-Less World and SHIFT to Professional Paradise:
Catalyst Consulting, LLC

Nancy Hickcox, MSN, RN, CNOR
Director Surgical Services and Anesthesia
UPMC Shadyside

Renee Dodge, MSN, RN, CNOR, RNFA
Director of Perioperative Services
Houston Methodist Willowbrook Hospital

Susan L. Hodgin, MSN, RN, CNOR
Manager, Neuro-Surgery
Vanderbilt University Medical Center

Kimberly Hoffman, BS, RN
Director, Clinical Performance Improvement
Medtronic Integrated Health Solutions (IHS), Americas
Gail M. Horvath, MSN, RN, CNOR, CRCST
ECRI Institute

Julie L. Hudson, MS, RN, CNOR, NEA-BC
Enterprise Administrator, Perioperative Services
University of Kentucky Healthcare

Philip Jaklich, MS, RN
VP Surgical Services, Spine & Joint
Sky Ridge Medical Center

Sherri Jones, MS, MBA, RDN, LDN, FAND
Improvement Specialist
UPMC Shadyside

Margo Karsten, PhD, MSN, BSN
Banner Health Northern Colorado Chief Executive Officer
Banner Health

Cindy L. Kildgore, MSHA, BSN, RN, CNOR
Perioperative Services Director
Vanderbilt University Medical Center

Beverly Kirchner, BSN, RN, CNOR, CASC
Chief Compliance Officer
SurgeryDirect, LLC

Susan Klacik, BS, AS, FCS, CHL, CIS, ACE, CRCST
Clinical Educator
International Association of Healthcare Central Services Materiel Management (IAHCSMM)

Jan Kleinhesselink, BSHM, RN, CPHQ
Chief Quality Officer
Lincoln Surgical Hospital

Jodi Koch, MBA, BSN, RN
Director of Perioperative and Endoscopy Services
Lehigh Valley Health Network

Dennis Kogan
CEO
caresyntax, Inc.
Dana M. Kopera, MBA, BSN, RN, CNOR
UPMC Altoona

Jane Kusler-Jensen, MBA, BSN, BSM, RN, CNOR
Specialist Master
Deloitte Consulting

Rory Langefeld, MPH
Administrative Director
Vanderbilt University Medical Center

Carmen Lester, JD, BSN, RN, CPHRM
Chief Clinical Officer
Lincoln Surgical Hospital

Teresa MacDonald, MSN, RN, CPAN
Nursing Practice Specialist
Massachusetts General Hospital

Denita Mckee, BSN, RN, CNOR
Medical Education Specialist
Olympus America Inc.

Jane McLeod, MSN, RN
Co-Founder
Capstone Leadership Solutions

Adam C. Messer, MPH
Associate Hospital Director/ VP Perioperative Services
Temple University Health System

Barbara E. Nosek, MHA
OR Business Manager
UPMC Altoona

Shane B. O'Neill, MSHA
Baylor University Medical Center

Carol Pehotsky, DNP, RN, CPAN, ACNS-BC, NEA-BC
Associate Chief Nursing Officer, Surgical Services and Senior Director, Surgical Nursing, Main Campus
Cleveland Clinic

Toni Perez, RN
PCM of Perioperative and Endoscopy Services
Lehigh Valley Health Network

Katelyn Printz
Manager, Human Resources Department
UPMC St. Margaret

Catherine Pusey, MBA, RN
ECRI Institute

Janet Quigley, MSN, RN
Nursing Director: Post Anesthesia Care
Massachusetts General Hospital

Margaret Ratcliffe, BS, RN
Director, Clinical Performance Improvement
Medtronic Integrated Health Solutions (IHS), Americas

Peter Rodney, MS, BSN, CNOR
Senior Director Perioperative Services
NYULMC's Hospital for Joint Diseases

Kenneth Rosenfeld, MD
Director of Perioperative Services
Stony Brook Medicine

John R. Rosing, MHA, FACHE
Executive Vice President
Patton Healthcare Consulting

Jennifer Schwartz, MSN, BSN, RN, CNOR
Regional Perioperative Director
Kaiser Permanente Southern California Region

Ann Seal, MHA, BSN, RN, CNOR, NE-BC
Assistant Vice President Perioperative Services - Metro
Carolinas Healthcare System

Patricia C. Seifert, MSN, RN, CNOR, FAAN
Perioperative Cardiac Consultant
Independent Cardiac Consultant

Rose O. Sherman, EdD, RN, NEA-BC, FAAN
Director, Nursing Leadership Institute
Florida Atlantic University

Ann Shimek, MSN, BSN, RN, CASC
Chief Nursing Officer
United Surgical Partners International

Keith Siddel, JD, MBA, PhD(c), CHC
Vice President
Universal Health Systems, Inc.

Allyson Silver, MPH
Hospital Executive Director, Surgical Services
Stony Brook Medicine

Ross W. Simon, BA
Senior Management Engineer
Beth Israel Deaconess Medical Center

Dennis Snow
Former Walt Disney World Company Executive
President, Snow Associates

Deborah Spratt, MPA, BSN, RN, CNOR, NEA-BC, CHL
Director, Surgical Services
Rochester Regional Health - United Memorial Medical Center

Cynthia Spry, MA, MSN, RN, CNOR, CBSPDT
Independent Clinical Consultant

Mary Jo Steiert, BSN, RN
Director of Clinical Operations
Lowry Surgery Center

Mary Szostakowski, MSN, RN, CNOR
Nurse Manager, Urology & Gynecology
Cleveland Clinic

Sue Tetzlaff, MHA, RN, RHIA, FACHE
Co-Founder
Capstone Leadership Solutions, Inc.

Lynne A. Thomas, BSN, RN, CGRN, CFER
VP - Education, Regulation, and Compliance
STERIS – Instrument Management Services

Gina Throneberry, MBA, RN, CASC, CNOR
Director of Education and Clinical Affairs
Ambulatory Surgery Center Association (ASCA)

Michael Tsang, MSW, MBA
Perioperative Business Manager
NYULMC's Hospital for Joint Diseases

Joe Tye
CEO and Head Coach
Values Coach Inc.

Dawn Vocke, MSN, MBA, RN, CNOR
Clinical Director Surgical Services
UPMC St. Margaret
Patrick Voight, BSN, MSA, RN, CNOR
Director
Deloitte Consulting

Anita A. Volpe, DNP, APRN
Director, Surgical Outcomes, Research, and Education
New York Presbyterian Hospital/Queens

Cy Wakeman
Author, Reality Based Leadership and The Reality-Based Rules of the Workplace and President and Founder
Reality-Based Leadership

Susanna S. Walsh, BSN, RNFA, CNOR, CSSM
Perioperative Services Manager
Vanderbilt University Medical Center

Pamela Werner, MBA, BSN, RN, CNOR
Sr. Clinical Consultant
Ansell Healthcare Products LLC

Brian Whorley, MBA
Director of Business Development & Planning
Boone Hospital Center

Miranda Woods, MS, BSN, RN, NE-BC
Vice President, Clinical Education
HCA East Florida Division
David Wyatt, MPH, BSN, RN, NEA-BC, CNOR
Associate Operating Officer, Perioperative Enterprise and Associate Nursing Officer, Surgery Patient Care Center
Vanderbilt University Medical Center

Ana Cecilia Zenteno Langle, PhD
Operations Research Manager
Massachusetts General Hospital
Networking Events

OR Manager Conference is your time to meet with perioperative leaders from around the country to swap stories and share leadership tools.
Don’t miss these fun networking opportunities with your colleagues:
OR Manager Conference 30th Anniversary Kickoff Party
Monday, October 2nd
The official kickoff to the OR Manager Conference is your first look at the vendors in the Exhibit Hall while enjoying hors d’oeuvres, drinks and time to connect with old and new colleagues.
Play the Build Your Dream OR Contest using the official mobile app while making new connections with your peers and solutions experts in the perioperative industry.
One ticket is included with your registration. Guest tickets are available through Registration.

Morning Motivational Meetup!
Tuesday, October 3rd
Enjoy some energizing snacks with fellow attendees to get you ready for all of Tuesday’s breakout sessions! This networking break will be in the Exhibit Hall, and will feature CEs presented by exhibitors and the OR Manager Conference Poster Gallery.
OR Manager Awards Presentation
Tuesday, October 3rd
OR Manager will be recognizing excellence in perioperative services management with the OR Manager Achievement Awards.
These awards are nominated by your colleagues and peers, selected by the OR Manager Conference Planning Committee and OR Manager Advisory Board, then presented to deserving individuals who have performed exceptionally in his or her management position.
Join your colleagues on October 3rd for the presentation of the Awards and to congratulate the winners, then continue the celebration in the Exhibit Hall during the Dessert Reception!



*The OR Business Manager of the Year Award will be presented at the 2018 OR Business Management Conference.
Meet the Poster Session Authors
Tuesday, October 3rd
You’ll have the opportunity to meet Poster Session authors, one-on-one, to get the answers to your questions on Tuesday, October 3rd.
Poster Sessions:
- Tuesday, October 3rd: 1:00 p.m. – 2:00 p.m.
- Tuesday, October 3rd: 3:30 p.m. – 4:30 p.m.
Refresh, Relax, Recharge! – Afternoon Break
Tuesday, October 3rd
Before the evening Keynote on Tuesday, be sure to recharge your educational vigor with healthy refreshments and bites, CEs presented by exhibitors, and visits to the Poster Gallery.
OR Manager‘s Night Out: Discovery Cove Beach Luau at SeaWorld
Tuesday, October 3rd
Get your flip flops ready and break out your sunglasses! The OR Manager Conference is hitting the beach!
Enjoy the Floridian sunset with your toes in the sand among your fellow colleagues in beautiful Discovery Cove at SeaWorld. Take your mind off the hard work you put in during the day and relax to some Caribbean music while enjoying dinner, drinks and entertainment – including live dolphins!
Tickets include a full buffet dinner, drinks, and dessert. For your entertainment, meet with our animal ambassadors to hold tropical animals, such as parrots and sloths.
Please note this reception is not included in your registration and must be purchased as an add-on ticket.
Continental Breakfasts and Networking Lunches
Discuss the latest perioperative developments over breakfast and lunch at OR Manager Conference. Breakfasts Monday-Wednesday and Lunch on Monday and Tuesday are included in all Value Package registrations.
Morning Walk and Talk
Wednesday, October 4th
Thinking, walking, and talking are all linked! Join your fellow attendees and a member of the OR Manager team for a “walk and talk” to get your day started on the right foot! This is our modern take on roundtable discussions. You’ll be able to get some exercise while meeting other perioperative leaders who share the same challenges as you. Bring questions raised during sessions, concerns from your OR, and hot topics to discuss with your peers.
Poster Gallery


View the Digital Poster Gallery Here
The OR Manager Conference Poster Gallery provides a forum for presenting completed research or in-progress research with preliminary results. It is an opportunity to present research, performance improvement projects, or clinical practice innovations visually using graphs, illustrations, or photographs. We strive to promote communication and collaborative research among nurses, provide a setting for exchange of information and lessons learned, and explore advances in perioperative clinical practice.
Posters in the Exhibit Hall
Posters will be on display in the Exhibit Hall during all Exhibition hours. The dates and times of Poster Sessions, during which poster authors will be available to answer any questions, are below.
Poster Sessions:
- Tuesday, October 3rd: 1:00 p.m. – 2:00 p.m.
- Tuesday, October 3rd: 3:30 p.m. – 4:30 p.m.
E-Poster Gallery
Beginning Monday, October 2, conference attendees may review the posters and take an online quiz for 10.0 CE credit hours. Login details will be distributed via email on October 2.
To access the 2016 ePoster Gallery and CE quizzes click here.
If you need assistance accessing the e-poster gallery, please contact Taylor Shaw at 301-354-1751.
POSTER ABSTRACTS
- An Innovative Approach to the Orientation of the Novice Nurse to the Operating Room
- Clinical Redesign: Improving Quality, Reducing Waste - Surgical Kit Redesign
- Code Stork
- Comparison of the Pressure Relieving Abilities of a Standard Operating Room Surface and a Standard OR Surface With a Static Air Overlay
- Creating Mindfulness through the Continuum of Care for Children with Special Needs
- Critical Service Line Merger: The Importance of Sustainability and Cultural Competency
- Dashboard Data Analytics Results in Optimal Patient Outcomes and Cost Savings
- Decreasing the Incidence of Peri-Operative Venous Thromboembolism
- Driving an Exceptional Pediatric Experience
- Effects of Knowledge Management in Hospital Nursing Organizations on Outcomes of Nursing Performance
- Green Means Go: Safer PACU Transitions
- Healthy Work Environment
- How Does Your Perioperative Leadership Fit into Your Organization’s Episode of Care Model Plan?
- Implementing a Culture of Safety in Surgical Services at UPMC St. Margaret
- Implementing a Tiered Huddle System to Gain Momentum in Continuous Improvement, Patient Safety, and Flow
- Improving Satisfaction Scores for the Pediatric OR: Utilizing a New Mobile Application to Enhance the Family Experience
- Improving Specimen Ordering Process
- Improving Throughput for Perioperative Services with Customized Patient Education
- Increasing OR Utilization Using Machine Learning and Mobile Technologies to Build Smart OR Block Schedules that Improve Access, Utilization, and Revenue
- Integration of BDV Clarity with Epic to Improve OR Documentation Workflow
- Keeping Connected: Using Technology to Engage, Educate and Monitor Your Patients to Improve Outcomes and Prevent Readmissions
- Leveraging Barcode Scanning to Analyze and Reduce Returned Items in the Perioperative Space
- New PACU Residency Program to Help Nursing Shortages in Recovery Rooms
- Nursing Resources for Quantification of Blood Loss: An Evaluation of Two Methods in Simulated Cesarean Delivery
- One Team/One Dream
- Operation Clean Air: The Initiation of Smoke-Free Operating Rooms
- Optimizing Outcomes of Sterile Processing Department Processes through Enhancement of Inter Professional Care Delivery in the Perioperative Setting
- OR Care Model Redesign
- Perioperative Services First Case Start Performance Improvement
- Positioning Beyond the Operating Room
- Promotion of Harm Prevention Metrics in the PeriAnesthesia Care Unit setting
- QI Initiative to Improve the Productivity of the Endoscopy Suite
- Reducing Flashing and the Need for Immediate Use
- Revitalizing the OR’s Unit Based Council: Improving the Present to Empower Nurses into the Future
- Robotic Surgery: Many Arms, Not Enough Hands
- South Carolina Surgical Quality Collaborative
- Surgical Patient Flow: Understanding the Challenges
- Team Stepps Implementation for Grant Medical Center Surgical Services
- The Bill-Only Implant Paperwork Pain; Streamline the Process in Your Surgery Suites
- The Impact of Team Training on Safety Culture in the Operating Room
- The Science of Cleaning Reusable Devices
- Total Cost of Ownership - Definition and Reasons to Consider
- UroLift System Treatment
- Using Data to Improve Performance: What’s Your Analytics Strategy?
- Utilizing Technology to Decrease Discharge Time, Improve Patient Experience, and Promote Family Centered Care in a Same Day Surgery Unit
- Why is it Important to Evacuate Surgical Smoke
An Innovative Approach to the Orientation of the Novice Nurse to the Operating Room
Authors:
Rosemarie Hevner, RN, MBA, CNOR, Professional Development Director, Perioperative Services, Tufts Medical Center
Patricia Wencis, BSN, RN, CNOR, Clinical Instructor, Operating Room, Tufts Medical Center
Abstract: Purpose/Objectives:
To increase the staff of perioperative nurses in the Operating Room of Tufts Medical Center and provide a comprehensive orientation to a large number of novice nurses utilizing the Periop 101 core curriculum orientation program.
Content:
An increase in surgical volume and the shortage of experienced Operating Room nurses prompted the leadership of Tufts Medical Center to commit to an aggressive recruitment and training program in late 2015. An extensive interview and selection process was conducted with the goal of beginning the program in January of 2016. During the first 5 months of 2016, a total of 14 novice nurses were recruited for this program. The Periop 101: the AORN core curriculum program was purchased for each novice nurse. The online modules provide the framework and theory of perioperative nursing. Our Clinical instructor provided daily reviews of the modules along with simulation lab experiences to prepare them for the Operating Room setting. At present we have a total of 19 nurses who have been trained utilizing Periop 101 and we are recruiting for an additional five nurses to begin the program in early Oct of this year. (2017)
Strategies for Implementation:
Our team consisted of a Professional Development Director for Perioperative Services and a Clinical Instructor for the OR. An interim Clinical Instructor was hired to assist in the didactic portion during the summer months of 2016.
The time frame of an orientation of a novice nurse to the Operating Room is typically, nine months to one year. The perioperative nurse is required to acquire the knowledge, skills and attributes of the OR environment, surgical instrumentation, equipment sterilization, and infection control during the first three months of orientation. The clinical rotation begins with a 4 week rotation in the scrub person role to reinforce many of the concepts from the education modules. Once this rotation is complete, the novice perioperative nurse begins the clinical orientation to the Circulating Nurse role. Guided by a preceptor, the novice nurse begins the journey to become the true patient safety advocate for the surgical patient. The traditional approach to orientation is to assign clinical experiences in the General Surgery service. Our first group of five nurses was assigned to the General Surgery service in March of 2016. As our second group of seven novice nurses, which were all new graduates, were nearing the completion of the didactic portion of their orientation; the challenge to provide clinical rotations in the General surgery service began evident. We had to consider placing the members of our second group into a more complex surgical case mix. The services of Orthopedics, Neurosurgery, and Ophthalmology were services that new staffs were rotated through after a solid foundation of perioperative nursing was attained. The placement of novice nurses in these complex services had never occurred previously in our OR. Additionally, our third group of two new graduate nurses joined the clinical setting six weeks later in July. The Clinical Instructor‘s complete focus included the coordination of daily assignments of the new staff, clinical oversight of the novice nurses and providing support to our experienced staff. This was the largest number of novice nurses that our operating room had ever supported. The experienced staff was challenged with teaching new staff every day for long periods of time. We maintained open lines of communication and provided flexibility with assignments whenever possible. The entire group of 14 novice nurses successfully completed the didactic portion of the Periop 101 core curriculum. At the six month mark of the program, an appreciation breakfast was held for the OR staff to thank everyone for their efforts supporting the new staff.
Outcomes:
The progress made by the entire group has been remarkable. Formative assessments are ongoing utilizing the core competency skill/procedure checklists provided by the Periop 101 program. The knowledge, skills, and attributes, (KSA), format allowed us to evaluate the novice nurses through actual return demonstration, simulation, and verbal explanation. There is also a self-assessment checklist which allows the novice nurses to track their progress throughout orientation. Examples of the core competencies include: surgical attire, preoperative nursing assessment, Universal Protocol, surgical counts, positioning the surgical patient, surgical hand hygiene, and hand off communication.
Our first group of 5 novice nurses completed their orientation in January of this year and a member was recruited for the Cardiac service, based on her achievements during this first year. The members of the second and third groups have become valued members of the Orthopedic team, the Neurosurgical team and the Ophthalmology service teams, after just six months in the operating room. The preceptors of these services have provided not only clinical expertise but supportive mentoring to new graduate novice nurses in the most complex surgical specialties of the OR. The consistency of working in small teams which is customary in specialty services has contributed to the positive outcomes of this program. A fourth group was brought on in Feb. of this year and we utilized the same strategy of assigning these novice nurses to the complex services of Orthopedics, Neurosurgery and Ophthalmology. We are in the planning stages for a fifth group in the fall of this year, which will bring our total to 24 perioperative nurses.
Successful recruitment and orientation of novice nurses require the commitment of the entire organization to support the training of the next generation of nurses. Utilizing the foundation provided by the Periop 101: core curriculum program, our department was able to onboard and train our next generation of perioperative nurses. Successful orientation programs require extensive planning, organization and extensive oversight to ensure that the novice nurses receive the clinical experiences to support the theory presented in the classroom.
References
Association of Perioperative Registered Nurses, Periop 101: A Core Curriculum, 2016-2017.
Clinical Redesign: Improving Quality, Reducing Waste - Surgical Kit Redesign
Author:
Sherri Witkins, BSN, RN, CNOR, Patient Service Manager Children's Perioperative Department, Yale New Haven Hospital
Abstract: Purpose/objectives: The goal of this QI initiative was to eliminate unneeded surgical instruments from the surgical field.
Content: Availability of correct surgical instruments is integral to operative success. However, the presence of unneeded instruments can result in wasted time, energy, human resources, and money. Most importantly, this mismatch can have a negative impact on a patient’s operative and anesthesia time. Conducted in at the Yale New Haven Health System (YNHHS), this initiative aimed to eliminate unneeded instruments used during surgical procedures, thereby decreasing operative time and increasing the likelihood of “correct” instrument availability.
Strategies for implementation
Sort and Simplify: The surgical technician and the Central Sterile Supply (CSS) representative presented each instrumentation kit to the surgeons to determine instrument utilization. The 80/20 rule was used to determine instrument retention. The 80/20 rule, states that, for many events, roughly 80% of the effects come from 20% of the causes. In this case, 80% of surgical cases use 20% of the instruments presented.
Sweep: The surgeons had veto power to eliminate an instrument if they felt it was required.
Standardize and Sustain: Following elimination, the CSS created new surgical kits that were then piloted. A survey was used to monitor usability of the revised kits and to ensure availability of required instruments.
Outcomes: Through multiple reviews, pediatric surgeons removed 28% of unneeded instruments. Over 84,000 instruments, annually, were removed from the sterilization process. Likewise, the GYN surgeons remove 19% of the instruments resulting in over 9,000 instruments, annually, being removed from the sterilization process. Ultimately, this work can be further extended to other surgical services and delivery networks.
Code Stork
Authors:
April Bennett, RN, Surgical Services Unit Nurse Manager, Bonner General Health
Joanne Filch, RN, OB Unit Nurse Manager, Bonner General Health
Tracy Autler, RN, Director of Quality , Bonner General Health
Pam Schillar, CRNA, Nurse Anesthetist
Abstract: Purpose:
Code Stork: An Emergency code at Bonner General for a laboring mother in distress who requires an emergency caesarean section and cannot wait until the Operating Room (OR) crew can respond.
Objectives:
Revise current code stork policy and implement a process improvement to achieve a positive outcome from an emergent situation.
To decrease decision to incision time to less then 30 minutes.
Content:
We are a Critical Access Hospital in rural North Idaho with a 4 room OR that does not have an in house call crew outside of the hours of operation. Many Pregnant women in North Idaho elect to deliver at home or outside of a medical facility. In a three month period BGH received two newborns born outside the facility that were in dire need of resuscitation. One of the infants survived, sadly the other did not. Internally, we experienced an intra partum fetal demise and questioned ourselves if the outcome could have been better if we were able to perform the necessary C-section faster.
Strategies of implementation:
Each night, the OR crew has a surgical suite set up for an emergency C-section should one occur during the night.
Equipment was standardize; Obstetricians decreased trays from 60 instruments to 9.
Medication trays were standardized and training for physicians and nurses were provided.
Multi disciplinary staff members were trained how to respond to a "Code Stork.
Training programs were created; including training the CNA's in the scrub tech role.
All Respiratory Therapists, ED nurses, and OB nurses were certified in Neonatal Resuscitation (NRP)
Identification badges that describe each role in a "Code Stork" were created and are assigned at the start of each shift.
BGH partnered with the Idaho Simulation Network to drill and simulate a "Code Stork" and pediatric trauma drill
Outcomes:
By continually practicing and training we are becoming more comfortable during every emergent obstetric situation. We hold a debriefing after each case, or drill, and identify any gaps or opportunities and grow with them. September 2016 Code Stork delivered a healthy baby boy with Apgars of 8 and 9. Decision to incision 10 minutes. December 2016 Code Stork delivered a healthy baby girl with Apgars of 6 and 9. Decision to incision 10 minutes. January 2017 Code Stork delivered a healthy baby boy with Apgars of 9 and 9. Decision to incision 7 minutes.
Our mission is to provide excellent care, and every healthy mother and baby is another example that we are succeeding.
Comparison of the Pressure Relieving Abilities of a Standard Operating Room Surface and a Standard OR Surface With a Static Air Overlay
Authors:
Debra L. Fawcett, PhD, RN, Director of Infection Prevention, Eskenazi Health
Lenora Maze, RN, CNS, CNS Surgical Care, Eskenazi Health
Abstract: A Pressure injury acquired in the operating room (OR) is not a new problem and is expensive with an estimated cost of between $44,000.00 and $128,000.00 each. It is imperative that we identify how well OR surfaces actually decrease or redistribute pressure for the surgical patient.
Questions:
1. There will be no difference in the interface pressures between a standard operating mattress and an operating room mattress with a static air overlay.
2. There will be no difference in the pressure redistribution of the standard operating room mattress and the pressure redistribution of the operating room mattress with a static air overlay?
A comparative descriptive design was used to identify differences between the standard OR surface and a standard OR surface with a static air overlay and was IRB approved. Redistribution properties were measured by mapping the sensing area and areas of contact with the surface. Over all peak pressure for each surface was measured via interface pressures. All participants were volunteers. Each volunteer provided BMI information before being tested on surfaces.
Data analysis was completed using a t-test to compare differences. Significance was set at .05. Forty volunteers participated. Each surface was measure for a total of six minutes. Four categories reviewed: overall difference, trunk, heels, and occiput. All categories measured were significant at .001mmHg.
Overall sensing area for redistribution on the OR surface was 483.09 compared to an increased surface contact of 533.91 with the static air overlay. Significance was at 0.05. Significance was reached for overall and trunk but not meeting significance for heels and occiput.
Creating Mindfulness through the Continuum of Care for Children with Special Needs
Authors:
Jennifer Simonetti, MSN, RN, CPN, Perioperative Nurse Educator, Magnet Program Director, Cohen Children's Medical Center
Sharon Goodman , MA, RN-BC, CPNP, Pediatric Service Line Nurse Educator , Cohen Children's Medical Center
Ann Shea , BSN, RN, Nurse Manager, ASU, PST, MRI, Cohen Children's Medical Center
Helen Landers , MSN, CPNP, Nurse Practitioner, Pre-Surgical Testing, Cohen Children's Medical Center
Francesca Weingartner , BSN, RN, CPN , Assistant Nurse Manger, PASU and PST, Cohen Children's Medical Center
Abstract: Statistically, one out of six children is diagnosed yearly with special needs. Some neurobehavioral diagnoses associated with children with special needs are, Autism Spectrum Disorder, Attention deficit disorder, and sensory integration disorder. Head banging, hand flapping, rocking, humming, and self-inflicted pain are common coping mechanisms utilized by children with special needs. These coping mechanisms increase in its intensity and frequency when in unfamiliar and over stimulating environments.
Children with special needs have a high need for medical care due to their multiple diagnoses and co-morbidities. Medical environments are often the antithesis for the promotion of healing and wellness with this vulnerable population and often results in aversions to future medical care. To provide quality care and prevent this aversion this institution developed and implemented an innovative exemplar program. Implementation of this program was intially in the in-patient area. Building on the in-patient success, the program was then expanded in phase two to incorporate the continum of care from physician/surgeon office, pre-surgical testing, ambulatory care unit, operating room, post anesthesia care unit and inpatient hospital stay.
Partnership with physicians and nurse practitioners in outpatient sites facilitated the initiation of this program. Through the use of education, awareness, desensitization, social stories, and planning this unique population was better prepared for their hospitalization and/or surgery. Press Ganey scores for “staff addressing personal needs” after implementation continued to increase and the average length of stay for children with special needs decreased from 4.5 days to 2.60, representing a 1.9 day decrease. Throughout the program patients are afforded golden opportunities to customize and individualize the care provided prior to entering into the hospital setting. This empowerment helped place control back into the patients and caregivers hands to ensure that they receive the individualized care necessary to meet all of their unique needs.
Critical Service Line Merger: The Importance of Sustainability and Cultural Competency
Author:
Ebony Mitchell, MSN, RN, RN II, Houston Methodist
Abstract:
The scope and size of healthcare's social and environmental impact represent tremendous opportunities for one of the most complex and continually transforming industries to improve cost efficiencies, patient safety, and quality. Sustainability, a competitive imperative, has been expounded upon by Lubin and Esty (2010) as being the newest business megatrend that balances and simultaneously optimizes the economic, environmental, and social impacts of organizational operations. Nevertheless, a unique challenge to effectively implement sustainability exists as organizational leaders attempt to effectively organize structures that align organizational, departmental, and individual activities around system wide strategic goals. Increasing mobility of the global population coupled with constantly changing demographics warrants recognition of the importance of ensuring some type of sustainable cultural competence in healthcare organizations. Without a sustainable culturally competent and inclusive healthcare environment at every level, patients and customers lack respect for providers and commonly verbally complain, and negatively rate their hospital experience on surveys, (Goodman, 2014). Mergers create opportunities to reposition organizations, however, the effectiveness of repositioning is only apparent when successful integration of physicians, clinical, and administrative teams as well as the cultures of different entities, effectively occurs at the service line level. This poster showcases how a successful merger is best accomplished and sustained when management engages in cultural competence and encourages such among staff.
Dashboard Data Analytics Results in Optimal Patient Outcomes and Cost Savings
Authors:
Linde Kramer, MA, BSN, RN, CNOR, NE-BC, CSSM, Director Operating Rooms, NYU Langone’s Hospital for Joint Diseases
Joan M Spear, MBA, RN, CNOR, CRCST, Clinical Consultant, JMS Consulting
Abstract: Bundled payments stipulated under the Centers for Medicare and Medicaid’s Comprehensive Joint Replacement program, provided the opportunity to improve planning and communication for every patient undergoing Joint Replacement in this facility. Physician leadership in the Department of Orthopedics was challenged by facility administration to deliver positive results of quality patient care using innovative concepts through the continuum of preoperative, intraoperative, and post-operative interventions. Nursing ceased the opportunity to embrace the same innovative techniques for preoperative planning huddles. Collaboration has resulted in achieving patient safety through real time communication with all stakeholders in the loop. In addition, a decrease in hospital costs using value based initiatives over a 4-year period was realized.
Overall impact includes detailed identification of equipment and supplies needed for each patient undergoing Joint Replacement, automated notification to all stakeholders including Sterile Processing, individual vendors, surgeons, and other departments within the facility. Projecting resources, both personnel and supplies, required is optimum for all stakeholders to make each patient procedure safe, organized, and streamlined. Prospective planning allows projection of financial expenses bringing all disciplines to the same level of resource optimization. This collaborative approach to patient care demonstrates the role of perioperative nursing in the continuum of care for the future.
Objectives:
- Identify two important contributions of preoperative patient planning huddles in total joint procedures.
- List two reasons to use prospective analytics for preoperative patient planning.
- Describe the value of having access to surgeon provided procedure information for preoperative planning in all areas i.e.; sterile processing, radiology, vendor/s involved, operating room.
Decreasing the Incidence of Peri-Operative Venous Thromboembolism
Authors:
Pamela O. Turner, MSN, RN, CNOR, Director of Nursing for Perioperative Services, NYCHHC- Jacobi
Maria Castaldi, MD, Assistant Professor of Surgery at Albert Einstein School of Medicine, NYCHHC- Jacobi
Abstract: Purpose
This collaborative pilot project was initiated through data received from the American College of Surgeons National Surgical Quality Improvement Program,(ACS NSQUIP) The NSQIP data immediately showed us we had a high rate of VTE’s in our surgical patient population.
Content
We formed a multidisciplinary focus group and used the ACS NSQIP best practice guidelines to develop our own protocol to identify and decrease these events. The protocol and tool were developed to evaluate all general surgical patients and to classify them either as: high, moderate or low risk for VTE’s.
The nursing staff in the Pre-Admission Testing area and Same Day Surgery unit, were educated in using the Caprini VTE Risk Factors Assessment tool during their pre-operative interview for the general surgery patients. Patients with scores of three or greater, reflecting moderate to high risk levels, prompts a discussion between the Surgeon or Physician’s Assistant and the patient regarding VTE prophylaxis (VTEP).
Strategies
Several strategies were utilized in making this project successful. The choice of using the Caprini Scale Risk Assessment form, the development of a standard script for all the providers to use in English or in Spanish and the development of a follow up telephone survey was conducted to the general surgery patients that received the VTEP.
Outcomes
The survey results are encouraging. Data through five months (Nov. 2016 – March 2017) gathered through follow up phone calls revealed the following results: 96% of the patients were contacted (179 /186), 89% deemed high risk, 94% of high risk received pre-operative Heparin. 99% (145/147) of the patients reported that the indications, risks and benefits of VTE were explained well or very well. 98.5% felt that safety and well-being is a priority based on peri-operative discussions. During this time frame there were no incidences of VTE.
Driving an Exceptional Pediatric Experience
Authors:
Deborah C. Gigliotti, MBA, RN, CAPA, LSSGB, Nurse Manager, Christiana Care Health System
Susan Pugliese, DDS, RN, Vice Chair Department of OMFS/HD, Christiana Care Health System
Abstract: Background [plan]: The Roxana Cannon Arsht Surgicenter delivers intraoperative dental care to over 350 children annually. Preoperative anxiety in the pediatric patient is a very common experience. Although all children are vulnerable to stress, preschool children and toddlers ages 1 to 6 years seem to be the most vulnerable. (Banchs et al, 2014). Preoperative anxiety manifests in different ways, from shivering and crying to fighting and trying to escape leading to a stressful experience for the patient, the parent and the healthcare provider. Interventions to reduce a child’s preoperative anxiety include use of distraction techniques and sedative premedication (oral midazolam). Though oral midazolam has strong safety and effectiveness records, studies show conflicting results related to quality of emergence, discharge times, and postoperative behavioral disturbances. (Rosenbaum et al, 2009). Distraction strategies have been shown to be effective at reducing preoperative anxiety in children. (Yip et al, 2011) Our medical director had a positive experience using motorized cars at another institution and as a result motorized cars were purchased as a more interactive distraction strategy.
Intervention(s) [do]: A remote control child’s motorized car and jeep were purchased in September of 2015 as optional strategies of interactive distraction to decrease preoperative anxiety in children ages 2 to 6 years. The cars supplemented personal DVD players, stickers, coloring books and paper for artwork already being utilized.
Results/outcomes [check]: For the purpose of this project anxiety level was measured by the need for preoperative oral midazolam. Prior to the car being purchased, 100 pediatric cases from February through April 2015 were reviewed for patients ages 2 to 6 years. The baseline data showed a preoperative sedation rate of 27%. After the car was introduced, 100 pediatric cases from October through December 2015 were reviewed for patients ages 2 to 6 years. The preoperative sedation rate after purchase of the car was 8%. Continued review of all cases of patients ages 2 to 6 years from January through August 2016 yields a preoperative sedation rate of 8%.
Conclusion [act]: A motorized car when used to augment the distraction strategies of DVDs, stickers, coloring books and participatory artwork decreased the preoperative sedation rate from 27% to 8%.
Effects of Knowledge Management in Hospital Nursing Organizations on Outcomes of Nursing Performance
Author:
Eunju Lee, PhD, RN, Professor, College of Nursing, Keimyung University
Abstract: Objectives: This study was conducted to investigate effects of implementation of knowledge management (KM) on outcomes of nursing performance.
Contents: Effective management of knowledge is very important to achieve strong organizational performance.
Knowledge management (KM) can only promote such organizational performance when members of an organization actively use and share their knowledge. The success or failure of KM depends on how effectively an organization’s members share and use their knowledge. Because KM plays a key role in enhancing nursing performance, identifying the core factors and investigating the level of KM in a given hospital are priorities to ensure a high quality of nursing for patients.
The study employed a descriptive research procedure. The study sample consisted of 192 nurses registered in three large healthcare organizations in South Korea. The variables of demographic characteristics, implementation of core KM factors, and outcomes of nursing performance were examined and analyzed in this study.
Outcomes: The relationships between the core KM factors and outcomes of nursing performance as well as the factors affecting the performance outcomes were investigated. A knowledge-sharing culture and organizational learning were found to be core factors affecting nursing performance.
Strategies for implementation: The study results provide basic data that can be used to formulate effective KM strategies for enhancing nursing performance in hospital nursing organizations. In particular, prioritizing the adoption of a knowledge-sharing culture and organizational learning in KM systems might be one method for organizations to more effectively manage their knowledge resources and thus to enhance the outcomes of nursing performance and achieve greater business competiveness.
Green Means Go: Safer PACU Transitions
Authors:
Amy Kohl, MSN, RN, CCRN, Nurse Manager, Christiana Care Health System
E. Chris Skinner, MSN, RN, CAPA, Assistant Nurse Manager, Christiana Care Health System
Lauren Speakman, MBA, BSN, RN, CCRN, Perioperative Practice Coordinator, Christiana Care Health System
Susan Volk, MSN, RN, CPAN, CCRN, Staff Development Specialist, Christiana Care Health System
Abstract: Background Information: Medication safety is often cited in literature, along with strategies to reduce medication errors. PACU uses an order set, tailored to the needs of the post-surgical patient, including high-risk opioid medications that are administered by carefully trained PACU nurses. Once PACU discharge criteria are met, the RN is expected to discontinue the orders in the electronic documentation system. Baseline data shows that only 76% of PACU order sets are discontinued prior to the patient leaving PACU. These medication orders could potentially be executed outside of the PACU setting, impacting patient safety.
Objectives of Project: Our goal is 95% compliance with discontinuing the orders before the patient leaves PACU, thus reducing the possibility of a patient receiving these medications.
Process of Implementation: The team utilized lean methodologies to identify barriers to the process and areas of opportunity. Verbal and email reminders were deemed ineffective. Visual cues were identified as an opportunity. The following strategies were implemented: 1.) RNs were asked to document on existing forms when orders were discontinued. 2.) Technology was leveraged within our electronic documentation system. Color changes from red to green were used when the event is set. 3.) An automated report was launched to track compliance with discontinuing the orders prior to the patient leaving PACU. 4.) Collected information was shared with staff.
Statement of Successful Practice: During the first twelve weeks of interventions, compliance increased by 15% to 91%. Acknowledging our goal of 95%, the team is continuing to improve the process through staff education and technology enhancements. Interventions to remind staff and enhance handoff communication related to discontinuing the PACU order set have improved compliance.
Implications for Advancing the Practice of Perianesthesia Nursing: Medication safety is improved by decreasing the potential for high-risk PACU medications to be administered outside of the peri-anesthesia environment. This initiative supports leveraging technology to create a culture of medication safety.
Healthy Work Environment
Author:
Carol Schneider, MSN, RN, CCRN, CPAN, Nurse Manager ENC and Menino PACU, Boston Medical Center
Abstract: Lateral Violence, bullying, and incivility continue to be serious issue in healthcare. It is an age old problem and unfortunately still remains prevalent in today’s healthcare workplaces. In July of 2015 the American Nurses Association (ANA) issued a position statement regarding incivility, bullying, and workplace violence.
The PACU I managed was no different from many of today’s academic medical center PACU’s. It is a busy high acuity unit with many changes happening constantly. Staff employee engagement scores demonstrated the need for improvement in areas of control over work decisions, and team respect. Observations of staff interactions demonstrated poor communication and conflict resolution skills. These are all factors that can negatively affect patient care and nurse engagement.
Along with my education colleagues, we planned to give the nurses in the PACU the tools to be skilled communicators. Three workshops were planned to provide knowledge and practice on skilled communication, conflict resolution, collaboration, and self-reflection. These workshops were mandatory for all staff, and included education, role play, and the creation of a unit code of behavior. The American Association of Critical Care Nurses Healthy Work Environment Toolkit was resourced for educational material.
The program ran over a year and evaluations by staff were overwhelmingly positive. Nurse engagement scores have improved, and staff have responded positively towards each other, and with interdisciplinary staff.
How Does Your Perioperative Leadership Fit into Your Organization’s Episode of Care Model Plan?
Authors:
Kathleen Wright, MSN, RN, Director, Population Health, Premier, Inc
Mary Pat Gilligan, DNP, Executive Director, Perioperative Nursing, TriHealth
Abstract: Under the new Episode of Care payment model, payments are structured to better align incentives to promote high-quality and efficient care. Healthcare providers are still paid fee-for-service (FFS), but they are held to a greater level of accountability for the total cost and quality of care delivered to their patients across the episode.
Perioperative Leadership recognizes that 2-3% of our population has the highest cost of care due to complex case management of comorbidities. Financial success will be based on clinical conditions that optimize patient care. For example, initiating optimization pathways and risk stratification related to diabetes, hypertension, anemia, sleep apnea, frailty and nutrition, can lead to better outcomes.
To help align with the episode of care, the Perioperative Leadership at TriHealth is moving towards a Perioperative Surgical Home (PSH) model of care, beginning with the decision for surgery and ending 90 days post discharge with a transition of care to the patient’s Primary Care Physician. The pilot patient population for this model of care is our elective colorectal patient population. Physician buy-in was achieved to roll out standardized enhanced recovery protocol orders (pre and post-op). Patients are contacted by the optimization nurses in the clinic within 48 hours of the referral.
At TriHealth, the Perioperative Surgical Home team has seen improvement in postoperative outcomes. Early implementation of the PSH model demonstrated a 7% improvement in readmission rates. The team has decreased length of stay improvements for the colorectal patients from 7.19 days to 5.79.
During implementation of the PSH model, a surgical site infection prevention bundle was embedded into the intraoperative navigator. This initiative has been instrumental in supporting a 64% reduction in surgical site infections at TriHealth for colorectal patients.
Implementing a Culture of Safety in Surgical Services at UPMC St. Margaret
Authors:
Dawn Vocke, MSN, MBA, RN, CNOR, Director, Surgical Services, UPMC St. Margaret
Mary C. Barkhymer, MSN, MHA, RN, CNOR, Vice President, Patient Care Services & Chief Nursing Officer, UPMC St. Margaret
Abstract: Changing culture is one of the most challenging endeavors an organization will encounter. Implementing a culture of safety in surgical services involved organizational commitment, multidisciplinary teams and focused interventions. Various strategies were used to engage staff and create an increased awareness in safety issues and processes. Five educational sessions were held including using evidence based practice, developing teamwork, employing a “just culture,” reporting events and debriefing. Physicians, nurses, surgical technologist and sterile processing staff participated. Motivational posters of staff were created along with a patient safety video involving staff. Through data collection and analysis, process errors were identified and remediated. Outcomes were communicated to the multidisciplinary teams and leadership. There has been increased staff and physician engagement in a culture of safety as evidenced by the results of the 2016 Culture of Patient Safety Survey.
Implementing a Tiered Huddle System to Gain Momentum in Continuous Improvement, Patient Safety, and Flow
Authors:
Stacey Wood, MSN, RN, CPN, Nursing Department Director, SDS/PACU, Children's Mercy Hospital
Kelly Stamps, MSN, RN, CNOR, Lean Quality Improvement Coordinator, Children's Mercy Hospital
Abstract: Purpose/objectives - Patient safety, efficiency and engagement are essential components in any successful healthcare institution. The development and implementation of a tiered huddle system within Children's Mercy Hospital’s Perioperative Services has drastically improved these components, supporting our patient-centered care model - “Patient-Centered: Every Action, Every Day.”
Content – Our tiered huddle structure allows for productive 2-way dialogue amongst the entire team. This process keeps everyone responsible for care before, during and after surgical procedures. Defined roles for communicating up and down tiers and keeps staff members are on the same page for the 65+ surgeries performed each day. Issues can be resolved at the most local level possible and escalated when necessary. Each day includes Tier 1, 2, and 3 huddles, as well as a hospital-wide Daily Safety Update huddle, allowing for engagement from front line staff all the way to hospital administrators. At the final tier representatives from 27 departments share updates on the daily operations of the hospital, with a primary focus on patient, family, and employee safety and patient flow throughout the organization.
Strategies for implementation – Initial steps included Daily Management System workshops and engaging frontline staff on what they need to know at the beginning of the day to be successful. Bringing the right people to the table at the right time to surface and escalate appropriate issue has allowed for collaboration, resource sharing, engaging front line staff, breaking down silos, focusing on patient, family, and employee safety, and patient flow throughout the organization.
Outcomes –By creating a structured avenue to surface concerns and bringing stakeholders together in this forum, we accomplish real time problem solving. This process has helped us learn about issues much earlier than we did before. This Perioperative Services tiered huddle structure has proven to be successful, improving overall safety, awareness, and engagement.
Improving Satisfaction Scores for the Pediatric OR: Utilizing a New Mobile Application to Enhance the Family Experience
Authors:
Kara Dobson, BSN, RN, PCCN, CNOR, Circulator, Orlando Health
Hamish Munro, MD, Pediatric Anesthesiologist, Orlando Health
Abstract: The use of mobile technology is increasing in healthcare. With pressure to be more transparent, hospitals are being urged to improve communication utilizing this technology, however the operating room is often excluded from this process. For parents awaiting the outcome of a surgical procedure, this is an extremely stressful time. Frequently they are left waiting behind the red line and in the dark. We sought to improve parental satisfaction and make the unbearable wait bearable. At Orlando Health Arnold Palmer Children’s Hospital, the EASE (Electronic Access to Surgical Events) app has been used for over 3 years to communicate to families while their child is in surgery. One-way messages, in the form of texts, pictures and videos are sent once the child is asleep, and approximately every 30-45 minutes thereafter. Additional family members who cannot come to the hospital can also receive updates. This mobile communication frees the family from the confines of the waiting room while still following, step by step, the progress of surgery. To determine if the use of the app influenced Press Ganey scores, we retrospectively analyzed eight communication and satisfaction related questions, comparing those who participated in EASE to those who did not. A total of 360 responses saw an average increase of 4%. A survey of the nurses sending messages revealed that this was a faster, more reliable, more efficient and more enjoyable method of communicating with the family than the traditional phone call or in-person visit. Our experience with the EASE app improved patient engagement for the nurses and increased Press Ganey scores, all the while improving communication, increasing satisfaction and transparency and reducing the anxiety of parents in the surgical waiting room.
Improving Specimen Ordering Process
Author:
Cherisse M. Davis, MSN, RN, Business Operations Director Perioperative & Trauma Services, University of Utah Health
Abstract: Purpose: Accurate anatomical pathology specimen test ordering can be a challenge for OR staff. Persistent issues with specimen ordering necessitated a practice change at our institution. A clinical task group comprised of scrubs and circulators were tasked to develop an improved practice standard. Principles from human factors research were applied to design and implement safety in our electronic record’s (EMR) specimen ordering process.
Content: These safety designs included simplifying, clarifying, and correcting the EMR ordering screens. Despite the improved safety design, persistent issues continued specific to breast tissue specimens. Staff missed documenting essential information required to calculate cold ischemic tissue time. In 2015, the College of American Pathologists revised the fixation rule requiring “tissue acquisition specimens should be immersed in fixative within one hour of the biopsy or resection” to avoid false negative results.
Strategies for implementation: Interventions included 1) Anatomical Pathology staff providing focused education to OR personnel, 2) proper specimen ordering and documentation training, 3) developing an annual competency, 4) conducting ongoing monthly audits to measure impact, and 5) providing staff individual feedback.
Outcomes: Initial 2016 data indicated a 97% breast tissue error ordering rate. Significant improvements were shown after the practice standard revisions were implemented demonstrating a sustained 97% correct breast tissue ordering rate by April 2017.
Improving Throughput for Perioperative Services with Customized Patient Education
Authors:
Catherine Awad, RN, MHA, CNOR, PMP, Process Improvement Manager, Perioperative Services, University of Chicago Medicine
Lisa Sandos, AS, Health Literacy Program Manager, Diversity, Inclusion and Equity, University of Chicago Medicine
Abstract: Project Purpose
One of the biggest reasons for case start delays in the OR is late or unprepared patients. Additionally, a significant number of cases are cancelled or delayed due to a patient eating prior to arrival, taking medication they shouldn’t, or arriving too late. The biggest cause of these lies with the instructions the patient receives prior to Surgery. At the start of this project, there were no standard instructions and the documents that were handed out are unprofessional and reflected bad on the institution.
Project Strategy for Implementation
We created a standard set of Pre-Surgery or Procedure documents for all surgery and procedure patients. These would be printed and given to patients at the time of scheduling. Documents needed to be customized and selected for each patient. Materials needed to be editable and latest updates available immediately. The materials need to be available through our EMR (EPIC) and be linked to our patient portal (MyChart). Materials must be available in non-English Languages.
Content
My Surgery Folder includes:
A. Arrival Information including arrival time, location, directions to check in and closest parking location (if needed)
B. My Surgery Guide
1) The Days and Weeks Before Your Surgery
2) Getting Ready – What to Expect
3) Personal Items at the Hospital
4) The Day Before Surgery
5) Checklist Before Surgery
6) The Day of Surgery
7) Getting Better After Surgery
C. Resources at University of Chicago Medicine
D. Travel Guide for Visitors
E. Procedure Specific Instructions
F. Food and Drink Instruction including bowel prep
G. Anesthesia Appointment Instructions including Medical History Form
Key Benefits or Outcomes of MyChart Integration
• Patient Satisfaction
• Ease of use for staff
• Integrated with existing processes
• Security meets HIPAA requirements and security standards
• Audit of communications to patients within EHR
• Utilization reporting
Increasing OR Utilization Using Machine Learning and Mobile Technologies to Build Smart OR Block Schedules that Improve Access, Utilization, and Revenue
Authors:
Sanjeev Agrawal, MA, President, Healthcare & CMO, LeanTaas
Ashley Walsh, MHA, Perioperative Business Manager, UCHealth
Abstract: Perioperative business managers feel significant pressure to meet the needs of surgeons and nursing staff while balancing operational targets (utilization, access, revenue). Current block schedule management approaches, which often rely on intuition and "tribal" rules, make it challenging to allocate OR time fairly and efficiently to surgeons. UCHealth solved this problem by leveraging predictive analytics and big data. In this poster presentation, we explain how we improved OR utilization and productivity with actionable dashboards, secure and convenient mobile block exchange, and smart block schedules that ensure the right surgeon gets the right OR at the right time.
Integration of BDV Clarity with Epic to Improve OR Documentation Workflow
Author:
Anna Hooker, MBA, HA, MS, Perioperative Business Manager, LMC SCLHS
Abstract: Purpose/objectives:
1. Improve perioperative workflow:
a. Decrease manual information input by RN in the OR
b. Decrease staff error due to labeling and information transferring
2. Eliminate HIPPA compliance issues:
a. Eliminate to patient information transferring to external devices such as flash-drive, CD
b. Access anywhere through secure VPN (Virtual Private Network)
3. IT (information technology) and EMR (electronic medical record) integration:
a. Customization of the interface improve staff satisfaction and efficiency in OR
Content:
Current state of our EPIC usage involves a lot of time consuming and unsecure practices including the inability to save videos and pictures taken during the procedure to the EMR. Pictures have to be printed and labeled by a nurse, then sent to the medial records, where it is scanned into the EMR. The video has to be transferred onto an external device such as flash-drive or CD.
Strategies for implementation:
1. Hardware installation (completed)
2. Software implementation within PACS, EPIC, servers (current stage)
3. Staff training on the usage of the hardware and software (partially completed)
4. Implementation of the new features which includes display of the on-line schedule changes, “time-out”, real-time physician remote view.
5. Physician training on the features such as media repository services, as well as usage of Clarity on other devices
Outcomes:
Implementation of the Clarity system will allow us to improve and streamline our current OR workflow. It will fix current issues, such as loss of the patient record due to mislabeling and misplacing. Additionally as we are striving to be an epicenter for a colorectal robotic program the Clarity system would allow us to share robotic surgery technique remotely through the teleconference function without physically bringing people into the OR.
Keeping Connected: Using Technology to Engage, Educate and Monitor Your Patients to Improve Outcomes and Prevent Readmissions
Authors:
Cindy Mahal, MS, BSN, BS, RN, CNOR, VP Surgical Services, Advocate Health Care
Flo Kiokemeister, MSN, BSN, RN, Project Manager, Advocate Health Care
Abstract: The purpose of the poster is to educate perioperative leaders on how technology can assist in the entire surgical experience. From improving outcomes to preventing readmissions utilizing simple smart phone technology that engages patients in mapping out their care pathways. We will highlight our colorectal program and the results of the project as well as the patients perceptive on the utilization of the technology. This interactive app engages the patient every step of the way from when to do the CHG bath, monitor hydration status to how much drainage are you experiencing from your ileostomy. By managing the patient pathway and building in simple algorithms we reduced the readmission rates as well as calls to the surgeon because we stayed connected with a smart phone. We experienced a reduction in LOS, readmission rate and a decrease in cost per case as well as an increase in patient engagement. See how utilizing main stream technology can help in your OR.
Leveraging Barcode Scanning to Analyze and Reduce Returned Items in the Perioperative Space
Author:
Sutton E. Murray, Financial Analyst, Massachusetts General Hospital
Abstract:
Purpose/Objectives: This process improvement effort seeks to identify and address the large number of items unused in surgical cases and returned with the case cart. We expect a reduction in the number of returned items to improve efficiency with inventory ordering and stocking, case pick, and budget health.
Content: To accurately gauge the scope of our returns problem, we created a methodology for barcode scanning returned items prior to being sent to Central Sterile Processing and Supply (CSPS). This took place over ten days that were staggered to ensure we captured scans for all days of the week (Monday through Friday) on two separate occasions. Supplies in the return bins were documented prior to being sent to CSPS from the OR. The returned items were then matched to the surgical case to identify opportunities for improvement.
Strategies for Implementation: Changes resulting from the returns scanning process will be reviewed and rolled out through the Operating Room’s End of Case Committee, in addition to regular communication and manager support. Scanning and re-evaluation will continue on a regular basis, with results being reviewed by a smaller committee.
Outcomes: Returns scanning and tracking is still an ongoing effort, however, based on the initial scanning session, we recommended removing the highest volume return items from surgeons’ preference cards. These are sent up often and seldom used, and are also available in room stock. We suggested returning high volume items that nearly all surgeons use, sutures and gloves, within the operating room. After placing these items in a bin post-case, the night staff will handle restocking to the room. Finally, the timeframe for the picking of items for cases was shifted to overnight to allow for an enhanced review of cases.
New PACU Residency Program to Help Nursing Shortages in Recovery Rooms
Authors:
Karen Edwards, MBA, BSN, RN, CNOR, Education Specialist II, Houston Methodist Hospital
Hong Tran, MBA, BSN, RN, NE-BC, Administrative Director Perioperative Services, Houston Methodist Hospital
Abstract: The Perioperative PACU nursing residency program is a formal five-month program developed to help alleviate nursing shortages in recovery rooms. This is a blended learning program that combines didactics, a variety of clinical rotations to include the ICUs, ongoing skills assessments, hands on experience in the simulation lab, and a presentation on a case study based on evidence based practice and the care of the post-operative patient.
Training is strengthened with the completion of the Essential Critical Care Orientation (ECCO) a Web-based program consisting of 11 modules with a total of 60 hours of testing and learning.
Program topics and content are evidence based, and come from the American Society of Perianesthesia Nurse (ASPAN) competency-based orientation. There were six nurses in the fall of 2015, and five nurses in the February 2016 PACU program. The ultimate goal is to train competent PACU nurses and retain them in the PACU environment.
Nursing Resources for Quantification of Blood Loss: An Evaluation of Two Methods in Simulated Cesarean Delivery
Authors:
Stella Nelson, RN, Clinical Support Specialist, Gauss Surgical, Inc.
Keng-Tsai Lin, BS, Research Associate, Gauss Surgical, Inc.
Karen Chavez, BS, Research Associate, Gauss Surgical, Inc.
Eric Hsieh, BS, Research Director, Gauss Surgical, Inc.
Abstract: Statement of problem:
Quantification of blood loss is recommended to facilitate early recognition of obstetric hemorrhage. The most common method uses gravimetric measurements where nurses weigh surgical sponges, estimate suction volume, and manually subtract non-blood components. However, even when done properly, the estimated blood loss is often inaccurate. A more accurate colorimetric method of QBL is available but its impact on nursing resources is unclear.
Methodology
We compared the nursing time required using the gravimetric method to the time required using a novel, colorimetric method. Twenty obstetric nurse volunteers from Santa Clara Valley Medical Center, San Jose, CA were timed as they processed laparotomy sponges (30) and canisters (2) to determine their blood content during a simulated cesarean procedure.
For the gravimetric method, nurses were asked to weigh sponges and visually estimate fluid volumes. Nurses then calculated blood loss using a worksheet. For the colorimetric method, nurses transferred, counted and imaged sponges using the novel mobile application (Triton System™, Gauss Surgical, Inc., Los Altos, CA) on a tablet computer (iPad). They visually estimated fluid volume in the suction canister and scanned the canister using a similar application. The blood loss estimate was generated by the Triton system. A paired t-test was used to compare the time required to complete QBL using the two methods.
Results
The time needed to obtain the gravimetric determination (363±82s) was significantly greater than the time needed using the image-based method (280±46s) (p <0.001).
Implications
The image-based method of estimating blood loss required less nursing time than the gravimetric method. Significant time savings were realized through the automatic calculations using the image-based method and implementation of this more accurate system should not be restricted by concerns about nursing resources or workflow.
Support for Research
Gauss Surgical, Inc. provided the Triton System used in this study.
One Team/One Dream
Authors:
Mary Pat Gilligan, DNP, CNOR, NEA-BC, Executive Director of Perioperative Nursing, TriHealth
Kathy Eten, BSN, Program Administrator Orthopedic Center of Excellence, TriHealth/Good Samaritan Hospital
Abstract:
Growing evidence suggests strong interdisciplinary collaboration and communication can improve clinical outcomes, reduce costs and impact both the patient and healthcare provider experience. Care teams that are unified and working toward shared goals work efficiently, maintain a safe environment and enhance satisfaction for both the patient and caregiver — while care teams that are working toward different goals or struggle to communicate open the door to unsafe practices and lead patients to believe their care was poorly coordinated.
The One Team One Dream Orthopedic Campaign is an innovative teambuilding approach focused to enhance a professional and collegial environment within the perioperative setting and to ultimately impact patient outcomes.
PLAN
Background Information:
• The Perioperative Department had experienced a turnover in staff resulting in many new staff members who were in orientation and unknown to the surgeons.
• A campaign was developed with a focus on communication, teamwork and patient safety and with an overall goal to improve satisfaction, foster relationships and change culture.
DO
A system was created and implemented for the staff and surgeons to rate each orthopedic case on a scale of 1 to 4 based on communication, teamwork, and patient and staff safety.
CHECK
Surveys identified some wins and challenges but the average rating did not fluctuate past 3.7 – 3.9 on a scale of 1-4 with 4 being completely satisfied.
CYCLE OF CHANGE
A method to electronically survey the staff was developed with new questions while still maintaining the same 1 – 4 scale. Only top box scores were reported along with Wins, Challenges and Staff/Surgeon recognition.
ACT
A standardized process is now in place to collect and report a Win, Challenge or team member recognition.
Results will continue to be monitored by the Campaign Leadership Team and the Orthopedic Operations Committee.
Operation Clean Air: The Initiation of Smoke-Free Operating Rooms
Authors:
Jane Lu, BSN, RN, Staff Nurse I, NYU Langone Medical Center
Maria Fezza, BSN, RN, CNOR, Nurse Manager, NYU Langone Medical Center
Mary Dobbie, BSN, RN, CNOR, CURN, Nursing Quality Specialist- Operating Room, NYU Langone Medical Center
Suzannah Sorin, MSPAS, PA-C, Physican Assistant Manager, NYU Langone Medical Center
Susan Titone, MSN, RN, CNOR, Nurse Educator, NYU Langone Medical Center
Abstract: Surgical smoke is a deadly byproduct of any operating room utilizing electrocautery and laser. Although professional organizations and literature have recognized inhalation and exposure as harmful to patients and preoperative staff, surgical smoke continues to remain a hazard. Consequently, an interdisciplinary team at New York University Langone Medical Center sought to improve safety by instituting a smoke-free program throughout the institution. Known as Operation Clear Air, the process change was based upon recommended practices, gap analyses, and education. The team consisted of Registered Nurses (RNs), Surgical Technicians (CSTs), a Certified Registered Nurse Anesthetist (CRNA), and a Physical Assistant (PA) to ensure that all operating room floors and specialties were represented. MD champions were conjointly recruited for each surgical service to assist with compliance, support, and scheduling of the educational sessions. Specifically tailored educational presentations took place for each audience group: RNs, CSTs, PAs, Anesthesia, and MD specialties. The sessions were a platform to bridge the knowledge deficit regarding the hazards of surgical smoke and increase familiarity with smoke evacuation equipment. Online modules developed by the Association of periOperative Registered Nurses (AORN) were assigned to RNs, CSTs, Clinical Perfusionists, and Surgical PAs to supplement the sessions. Data was then collected on total surgical smoke evacuation supply usage prior to and after the initiation of the program, as a means to monitor compliance. The total usage has more than quadrupled since the start of education, and ongoing weekly audits in all operating room suites have occurred to ensure that staff understood the proper handling of all equipment. Additional unit based education continues daily and is a constant reminder that safety is the responsibility of all preoperative staff members.
Optimizing Outcomes of Sterile Processing Department Processes through Enhancement of Inter Professional Care Delivery in the Perioperative Setting
Authors:
Judy Montello, BS, RN, Director of Perioperative Services, Childrens Hospital
Bridget Viloria, RN, CNOR, Manager of Perioperative Services, Childrens Hospital
Abstract: Background: Enhancement of interprofessional care delivery has a direct effect on positive patient outcomes. Today’s health care organizations need to be diligent in efforts to improve interprofessional care delivery in the perioperative setting. Ensuring interprofessional care delivery in the perioperative setting requires a multidisciplinary collaboration between all members of the surgical team, which also includes personnel in the Sterile Processing Department (SPD). A multidisciplinary collaborative approach can improve relationships and communication between personnel which can contribute to reducing errors and misunderstandings while increasing morale, productivity and operations. Strategies include a team focus on improving interdepartmental communication, fostering teamwork and positive relationships, improving decontamination processes, reducing instrument set errors, and ensuring compliance with policies that are based on the most current evidence available.
Purpose: To improve efficiency and work quality in the SPD, the perioperative team was trained on a new instrument cleaning process. Competent SPD staff trained perioperative nurses and surgical technicians on the new instrument cleaning process over several weeks while the SPD Coordinator verified competencies. The same multidisciplinary collaborative approach helped improve work stations, instrument sets, instrument count sheets and communication.
Methods: In December 2016, a multidisciplinary team formed, including perioperative nurses, Surgical Technicians and Sterile Processing personnel to quickly and effectively improve collaboration for safe and quality patient care. Using a Plan, Do, Study, Act methodology, changes were made to both sterile processing procedures and staff-related operational procedures. Patient safety concerns that included the Sterile Processing Department were compared during implementation from December 2016 to June 2017 to determine statistical significance of the strategies implemented by utilizing a huddle instrument.
Results: The following practices were instituted:
- Improvement & standardization of the workflow in decontamination by prioritizing sets to be cleaned, educating and ensuring all instruments are appropriately processed through the three-sink method of soaking, cleaning and rinsing.
- Mandated competency for all staff in the decontamination area by each demonstrating the instrument cleaning process.
- Improved work stations by organizing and stocking each station with uniform items needed for processing.
- Improved instrument sets by removing or adding instruments to allow for unnecessary instrument reprocessing and unnecessary utilization of individual peel packed instruments.
- Revised instrument count sheets to include a standardized form to improve ease of documentation by SPD personnel and to improve the instrument count process in the surgical suite.
- Updated process improvement forms to include pertinent surveyor questioning information and organized logs by separating documentation for each sterilizer to improve tracking.
- Discussed and purchased new equipment needed for process improvement.
- Changed SPD leadership by replacing a surgical technician with a registered nurse to provide administrative support and to function through professional-level administrative duties.
- Implemented SPD environmental rounds checklist to ensure a safe environment.
- Staff was restructured by changing PRN staff shifts to accommodate workload and additional staff was hired to accommodate the added processes in the decontamination area.
- Implemented weekly staff meeting including perioperative nurses, Surgical Technicians and SPD staff.
- Implemented a daily communication huddle instrument with the SPD staff to measure patient safety events and improve positive patient outcomes. Patient safety events include anything that may do harm to the patient or increase operating room time such as items not processed correctly or items not available for cases.
Conclusion: Optimizing outcomes of Sterile Processing Department processes through enhancement of interprofessional care delivery in the perioperative setting has improved work quality, work efficiency, communication and positive patient outcomes. By implementing improved strategies utilizing a multidisciplinary approach, the SPD experienced a 91% reduction in SPD patient safety events.
OR Care Model Redesign
Author:
Laura Licea, DNP(c), RN, CNOR, CSSM, HACP, OR Clinical Manager, Long Beach Memorial Medical Center
Abstract: Purpose/Objective
The purpose of the OR Care Model Redesign is to ensure the delivery of the right care at the right time and the right place with right resources. In pursuit of perfect care, redesign of the care model must include: quality patient centered care, coordinated care (patient/family/care team), and financial resilience. The OR Care Model Redesign was developed by Lean mythologies to ensure that all staff and management are clear on their roles and responsibilities and demonstrates ownership through accountability and visibility of processes. Right staff at the right time in the right operating room.
Learning objectives for the OR Care Model Redesign were chosen with the mission, vision, and values of the organization. The Mission of the organization is to improve the health and well being of individuals, families and our communities. The vision is for exceptional people, extraordinary care, every time. The values of the organization are: Integrity, Accountability, Best Practices. Compassion and Synergy. Therefore the learning objectives for my project will be the following:
- Quality and Value- Create standard work for all staff members of the operating room to maximize patient safety and reduce waste
- Market differentiation & Growth- Increase surgeon preference to use our hospital by streamlining the OR processes
- Financial Resilience- Reduce overtime, improve staff utilization to maximize productivity. Ensure there is a shared vision and commitment about how to optimize the flow and functions of the Perioperative Services.
- People & Culture- create clarity of roles and responsibilities for operating room staff and front line management. Ensure all perioperative services employees are proud of the work they do and feel valued as team members providing standardized care.
The strategies for implementation will include: posters (visuals), in-services during staff meetings and a complete packet that will detail their role, their assigned task by time of day and standard workflow for each role. The outcome for the OR Care Model Redesign is to ensure the perioperative team is accountable for meeting the Perioperative KPI’s. Optimize the surgical schedule through better utilization of rooms and staff. Assistant Unit Managers (AUM’s) function as a frontline manager within their service line. AUM’s will have accountability for the staff scheduling. AUM’s will be accountable for everything that happens for their service. All staff members follow standard work and established guidelines.
Perioperative Services First Case Start Performance Improvement
Authors:
Cynthia Rosevelt, RN MSN CNOR, Clinical Director Surgical Services, St. Luke's University Health Network Quakertown
Michelle Jacobs, RN, CNOR, Clinical Coordinator Surgical Services, St. Luke's university Health Network Quakertown
Abstract: Procedural and operating room time is costly with efficiency of this time crucial to revenue earning capabilities, patient safety and marketing ability with customers and key stakeholders. Operating room time is governed by a block schedule with defined time periods assigned to specific Physicians/Surgeons to perform surgery/procedures. Starting on time is crucial to the success of the daily operations in regards to costs, patient satisfaction, staff satisfaction and patient safety. With the implementation of EPIC electronic documentation and the ability to run EPIC validation reports, it was discovered first case of the day was starting 20% on time. As a performance improvement initiative, this project was implemented with the intended goal to have first case starts begin on time at least 80% by January 2017. A multidisciplinary approach was utilized to address efficiency concerns, reasons for delay, and interventions for improvement and time management. The full spectrum of care for a surgical patient was explored and evaluated beginning with Preadmission testing and ending with discharge of patient addressing all areas of care the patient experienced that influenced first case start times. The success of this performance improvement initiative was greatly due to the full engagement of all stakeholders to include, staff, Physicians/Surgeons, Anesthesia providers, ancillary departments and Leadership team. By January 2017 first case procedures started 94% on time at the St. Luke’s Quakertown operating room.
Positioning Beyond the Operating Room
Authors:
Sheila Capasso, MSN, RN, ACCNS-AG, CAPA, Advanced Practice Manager, The Miriam Hospital
Kathy Buckhaults, MS, RN, CNOR, Clinical Manger OR/ PACU, The Miriam Hospital
Diane Ferri, MSN, Clinical Nurse Manager Surgicenter OR/ PACU, The Miriam Hospital
Abstract: Purpose/ Objectives:
The purpose of this project was to reduce the incidence of Hospital Acquired Pressure Ulcers (HAPUs) in in all surgical patients.
Content:
The National Pressure Ulcer Advisory Panel (NPUAP) defines pressure ulcer as a “localized injury to the skin and/or underlying tissue usually over a boney prominence, because of pressure, or pressure in combination with shear.” Identifying patients who are at risk for developing intraoperative pressure ulcers is the first step toward preventing HAPUs.
In 2008, the Centers for Medicare & Medicaid Services (CMS) ceased reimbursing health care facilities for the treatment of HAPUs. According to NPUAP, pressure ulcers that originate in the OR account for up to 45% of all HAPUs.
With the incidence of pressure ulcer development in the perioperative setting, there were opportunities to educate our staff that work in the postoperative setting on identifying areas of localized injury or risk areas, due to length of surgery and position of patient.
Strategies for implementation:
In 2016, we developed a picture tutorial on surgical positions, to include specialty beds and positioning devices. The nurse in both the OR and PACU were educated about the pictures with and explanation of high risk points. The plan was for the OR nurses to share the pictures at the bedside with their PACU counterpart, during report.
The advanced practice manager met monthly with the pressure ulcer committee to review any HAPUs that could have been associated with the OR. That information was brought back to the leadership team.
We then brought the picture tutorial to the unit councils on our associated surgical floor, and the pressure ulcer committee.
Outcomes:
The pictures allowed the PACU and in-patient nurses, a better understanding of where to concentrate skin observation based on positioning.
Promotion of Harm Prevention Metrics in the PeriAnesthesia Care Unit setting
Author:
Dekeisha Howard, RN, MSN, NE-BC, PACU Nurse Manager, Children's Hospital of Philadelphia
Abstract: Purpose: The purpose of promoting harm prevention metrics in a PeriAnesthesia setting is to gain bundle compliance and surveillance of key quality indicators. The implementation of leadership oversight is to increase bundle compliance and decrease harm.
Content: Harm Prevention and bundle compliance are key metrics monitored in the inpatient setting. However, there is limited focus on procedural areas. To influence compliance, buy in and sustainment of harm prevention in the PACU we aligned a leadership nurse with a harm prevention champion to change the culture within our team.
Strategies for implementation: To implement this process each leadership team member became familiar with the harm prevention indicator, bundle and goal to achieve by year end. Each champion joined forces with the leadership nurse to review data, develop strategies to decrease rates and increase bundle compliance as well as educate and communicate our success monthly.
Outcomes: The collaboration and partnership amongst the teams led to an increase in harm prevention engagement as well as understanding of the indicator in relation to a procedural area.
QI Initiative to Improve the Productivity of the Endoscopy Suite
Author:
Rozanna Penney, Director of Perioperative Services, Heywood Healthcare
Abstract: The primary objective of this QI initiative was to improve the productivity of the endoscopy suite and thereby increase revenue, improve patient satisfaction and access to care.
Content: Prior to the implementation of this QI initiative, productivity in the endoscopy suite was limited by a multitude of operational challenges. As a direct result of the unit’s limited clinical productivity, first-available appointments for elective procedures were typically scheduled more than 120 days out. This four-month procedural delay resulted in referral loss, patient dissatisfaction, and directly contributed to a “no-show” rate up to 15%. Appointment reminder letters were sent via the US Postal Service 30 days prior to the procedure. On the day of the procedure, patients were admitted to the Surgical Day Care (SDC) Unit in advance of the procedure, admitted to PACU immediately after the procedure and subsequently returned back to SDC for discharge.
Strategies for implementation: With an initial focus on time wasted during the visit, the process was changed so that patients could be discharged to home directly from PACU. This resulted in enhanced continuity of patient care, greater availability of SDC beds and RN staff and expedited admission process. The procedure length was objectively quantified and booking times were adjusted accordingly. Automated as well as in-person reminder phone calls were implemented. A cancellation list identifying patients interested in having their procedure sooner was created and aggressively referenced whenever notice of a cancellation was received. The schedule was reviewed daily going one week out.
Outcomes: This QI initiative resulted in enhanced performance on several operational metrics: the average patient length of stay post procedure decreased by 36 minutes; the first-available appointment for elective procedures decreased from an average of 120 days out to 30 days out; the “no-show” rate decreased by 38%; overall case volume increased by 9%.
Reducing Flashing and the Need for Immediate Use
Authors:
Eleonora Shapiro, DNP, MHA, CNOR, NEA-BC, Associate Executive Director, Lenox Hill Hospital Northwell
Beata Mastalerz, DNPc, MSN, CNOR, Sr. Perioperative Director, Lenox Hill Hospital Northwell
Abstract: Purpose/objectives:
Association of Perioperative Registered Nurses (AORN) recommends that immediate steam sterilization (IUSS) should be kept to the most minimum use and should only be used in immediate urgent situations where no other option but to sterilize exists (AORN, 2017). In 2014 at our 22 operating room facility our flash rate was 4% percent. A huge improvement from 2012 where the flash rate was 15% percent.
Objectives:
Our objective was to reduce the flashing of any kind to less then 1% percent.
Strategies for implementation:
-Multidisciplinary meetings to discuss the possible causes for the immediate use sterilization needs. The meetings included the staff and the managers from Central Sterile Department and the operating room.
- Historical data for the previous 12 months compiled to understand which instruments most often were sterilized for immediate use and what were the reasons for those needs.
- Reporting system created to monitor instruments sterilized for immediate use and the reasons.
- Included IUSS report in the daily multidisciplinary management huddles to discuss the instruments sterilized for immediate use during the previous day.
- Staff education performed to ensure clear and timely communication pathways before each IUSS. The OR staff was advised to notify respective nurse manager, who then if needed called for the huddle with the SPD team, vendors or physician to evaluate if the substitute instrument/s could be used. Reminder signs posted on each autoclave.
- Based on the information compiled in the historical reports additional instruments were purchased
- Instrument tray paper wrappers evaluated and changed to thickest material available
- Corner protectors and tray liners in addition to the outside plastic trays (to assist when moving the tray and for storage) implemented.
- Shelf liners implemented in all storage areas
- Stocking of the trays minimized
- Additional storage created by eliminating instrument trays no longer used but stored on the shelf
- Physician named trays changed to the universal service/procedure related trays
- Physician preference card updated
- Consistent monthly reporting to the staff and constant collaborative apporoach to increase vigillence
- Celebrated the wins
Outcomes:
Consistent for over 12 months IUSS rates below 1% for large tertiary hospital performing over 16 000 procedures annually.
Revitalizing the OR’s Unit Based Council: Improving the Present to Empower Nurses into the Future
Author:
Nicole M. Schliecker, MSN, RN, CNOR, Unit Director, UPMC Shadyside
Abstract: In 2010, our hospital achieved Magnet designation supporting a strong culture of shared leadership. As a result, each nursing unit was charged with creating a unit based council (UBC) with frontline nurses and support staff at the helm. The Operating Room (OR) had a UBC for quite some time. Due to intermittent OR Unit Director turnover, the UBC had evolved into an ineffective group with little outcomes, frequent negativity, and lack of organization. With hire of a new OR Unit Director in May 2016, the UD set out to revitalize the UBC with the aim to create a more effective shared leadership structure.
To accomplish this, the OR partnered with an Improvement Specialist to design an organized improvement plan to include a UBC Toolkit. The hospital’s global shared leadership by-laws were used to develop OR UBC written guidelines. Standard UBC meeting dates and times were set based on staff schedules. Current OR UBC membership was dissolved and started new by requiring interested staff to complete a formal application. All OR staff positions were encouraged to apply with intent of broadening the scope of positions represented. Elections were held for UBC Chair and Co-Chair with staff vote. Templates were created for meeting agendas and minutes for consistency. The newly revitalized OR UBC began meeting in December 2016.
After 4 months, the new UBC was evaluated by conducting a survey of current UBC members and all OR staff. Survey results revealed 75% staff overall felt the UBC is making progress; 73% staff is pleased with the current UBC, and 93% UBC members are pleased serving on the current UBC.
With its success, the UBC toolkit has been shared with all of our hospital nursing units. As the revitalized OR UBC continues to improve over time, NDNQI nurse satisfaction scores will be monitored.
Robotic Surgery: Many Arms, Not Enough Hands
Author:
Carrie Walters, Director of Nursing North TX Division Surgical Services, Baylor Scott & White Health
Abstract:
The purpose of this project was to generate innovative thinking about nurse staffing to assist OR leaders in determining a safe and cost effective staffing model for robotic surgical procedures. Content Traditional staffing patterns in the OR are not congruent with meeting the demands of today's complex robotic surgical procedures. Operating room employees and surgeons were growing increasingly dissatisfied with overall case workload and associated inability to meet efficiency metrics for robotic procedures. Attempts to discover patient and case acuity tools specific for use in the operating room were unsuccessful. Expert perioperative nursing staff used evidenced based information on core elements of perioperative nursing practice to develop a human resources time and motion study tool. This tool was used in conjunction with the NASA Task Load Index to observe and analyze the workload required of registered nurses assigned to robotic surgical procedures. Strategies for implementation Information gained from this study enabled development of a staffing model for robotic surgical procedures. The process used has implications for developing staffing models for other surgical procedures. Outcomes Data from a total of 25 robotic surgical procedures helped to identify the number of and most cost effective combination of personnel required to safely and effectively care for patients undergoing robotic surgical procedures. Key times of need for additional support resources were also identified to facilitate improved surgical start times and turn-over times.
South Carolina Surgical Quality Collaborative
Authors:
Larry Adams, MSN, MBA, RN, Program Director , SCSQC
Mark Lockett, MD, Program Surgical Lead, MUSC
Abstract: Background: Regional surgical quality Collaboratives are improving surgical quality and cutting costs by building regional relationships that leverage information sharing to improve outcomes through nurse abstracted case reviews.
Methods: The South Carolina Surgical Quality Collaborative (SCSQC) is a new regional surgical quality Collaborative focused on improving general surgery outcomes in South Carolina. It is a joint effort which brings together the skills and resources of Health Sciences South Carolina, the South Carolina Hospital Association, The Medical University of South Carolina, and The Blue Cross Blue Shield of SC Foundation to create a web-based data collection system to provide real time outcomes data to participating surgeons, as well as establishing a supportive network for sharing best practices and promoting data driven quality improvement.
Results: Members of the SCSQC have abstracted over 10,000 general surgery cases from eight participating hospitals. These facilities are spread across the state of South Carolina and range from large academic referral centers, to small community hospitals. Monthly conference calls and quarterly face-to-face meetings occur with site Surgeon Leads, site Surgical Clinical Quality Reviewer, and Collaborative leaders. Each site is pursuing a quality improvement project addressing issues identified from analysis of their initial data.
Conclusions : The South Carolina Surgical Quality Collaborative is a new regional surgical quality Collaborative which leverages multiple state resources, builds on the successes of similar Collaboratives in Michigan and Tennessee, with the goal to improve the quality and value of general surgical care for South Carolinians.
Support for Research : The SCSQC is funded by The Blue Cross Blue Shield of SC Foundation for the first three years. After the three-year period, SCSQC will work with Blue Cross Blue Shield of SC to transition to the operational budget to continue improving surgical quality beyond the eight starter sites.
Surgical Patient Flow: Understanding the Challenges
Authors:
Jan Thode, BS, RN, Periop Consultant, Lucile Packard Children\'s Hospital - Primus Healthcare Consulting
Penelope Boyd, MSN, RN, CNOR, Periop Consultant, Lucile Packard Children\'s Hospital - Primus Healthcare Consulting
Abstract: 1. Purpose/objectives
• To utilize data analytics to drive process re-design to improve throughput in the Perioperative environment;
• To reduce non-value-added activities that negatively impact the patient, staff and surgeon experience;
• To reduce OR Delays and Patient wait times in the Preop phase.
2. Content
• Surgical Patient Flow map;
• Cascading Impact of First Case Delays;
• Analysis of Delays in Preop Flow;
• Analysis of Delays in Holding Area
3. Strategies for implementation
• Initial stage of the project focused surgical outpatients and AM admits in the Main OR & Ambulatory Procedure Unit from April 2015 to March 2016;
• Current state flow was mapped after shadowing patients, observing the processes in pre-op, interviewing the nurses, patient care managers, and anesthesiologists;
• Timestamps from the Epic EMR were overlaid into the patient flow map, then the data was analyzed to identify the impact of various types of common delays, which uncovered considerable variability in staff, anesthesia and nursing practice;
• The two primary areas of focus for this project were availability of interpreters, as well as completeness of required preop documentation (orders, consent, H&P). and reducing wait times in Preop Holding.
4. Outcomes
• Majority of delays caused by factors external to the OR, missing Preop paperwork, lack of interpreters and log waits Holding;
• The 20-minute call out to move the next patient to Preop Holding was often being made too far in advance and between case turnover, especially for complicated cases was not being take into consideration, causing the LOS in Holding to balloon to 30 minutes or more;
• The need for additional interpreters was clearly identified and addressed with Interpreter Services;
• Service/Surgeon specific data on incomplete elements of the required Preop documents (Orders, Consent, H&P) were shared with Division Chiefs
Team Stepps Implementation for Grant Medical Center Surgical Services
Authors:
Valerie Seus, MBA, BSIE, BSN, RN, CNOR, Director of Nursing, OhioHealth Grant Medical Center
Cassandra Merkle, MSN, BSN, RN, Director of Nursing, OhioHealth Grant Medical Center
Abstract: Purpose/Objective: Teamwork, Communication and Patient Safety are essential to excellent patient care in the peri-operative environment. Ineffective and/or incomplete communication and staff inability to advocate have lead to increased safety events and a decrease in the culture of safety. With the implementation of the Team Stepps® methodology, we have improved Teamwork, Communication and Patient Safety within peri-operative services at OhioHealth’s Grant Medical Center.
Content: The initial project, Physician-led Time Outs, provides the necessary structure to perform an accurate and optimal Universal Protocol. All staff in the OR suite have defined roles and scripted information to report, and the proper pause is enacted when the surgeon calls the room to attention to begin. Everyone in the suite is introduced and is focused on the information given. Graphical data will be displayed to reflect results of Associate Safety surveys; feedback sessions with staff, physician and administration; before and after safety and burn-out assessments; and initial project results.
Strategies for Implementation: It is vital when undergoing a major culture shift that front-line staff play a primary role in the development and initiation of change. In order to find the root cause and most impactful areas of change, feedback sessions were held with staff and physicians at all levels. With safety as the primary area of concern the change team highlighted several initiatives, designed the training, and lead education sessions for hundreds of associates about the Team Stepps® tools selected.
Outcomes: By educating the entire peri-operative area about the tools and methodolgies of Team Stepps®, we have begun to ensure everyone communicates with the same language. The Physician-led Time Out has been implemented sucessfully and is being performed with great proficiency. This is only the beginning of a long-term culture change, but it is well under way.
The Bill-Only Implant Paperwork Pain; Streamline the Process in Your Surgery Suites
Author:
Jim Ferch, M.S. Contract Administration, Director Supply Chain, Marshall Medical Centers
Abstract: Introduction:
The pain with bill-only procedures within our operating rooms and cath labs is the manual processes required in capturing the usage and maintaining that data in our charge masters, item masters and patient billing. We struggle with all the touch points associated with these high-end procedures and we treat them with the respect of a slip of paper and pencil to document and capture the devices implanted. Briefly, this white paper identifies the pain points within existing manual processes and illustrates the advantages of streamlining all those touch points with the SimplifyOR iOS app.
The Pain Points:
Our implant write-ups get overlooked, posted late or misplaced.
Our item master costs and charge master charges are not current.
Our charge numbers posted don’t reflect the devices implanted.
Our item master pricing isn’t aligned with our contract pricing.
Our recall of usage may differ from vendor rep for the procedure.
Inaccurate usage and cost capture can lead to billing issues.
Our current processes are not aligned our EHR goals.
The application will aid three sets of processes:
1.Preparing for the surgery.
2.Recording and approving of consumption and costs
at the OR during the procedure.
3.Minimize dispute resolution leading to timely
issuance of P.O. and invoice.
Nursing: A Precious Resource
In an era of serious health care worker shortages, particularly when OR Nurses are needed, we must use our caregivers’ time as efficiently as possible. For the various stages of care of a typical patient, paperwork adds at least 30 minutes to every hour of patient care provided and, in some settings, adds an hour of paperwork to every hour of patient care.
The burden is simply too heavy - at the expense of patient care.
The Impact of Team Training on Safety Culture in the Operating Room
Authors:
Anna DaSilva, DNP, MBA, RN, Director, Periopertive Services, Milford Regional Medical Center
Stephanie Colman-Brochu, DNP, MSN, RN, Director Nursing Informatics, Milford Regional Medical Center
Paul Darcy, MD, Chief of Anesthesia, Milford Anesthesia Associates
Angela Kulesza, DNP, NP-C, Associate Professor of Nursing, Regis College
Abstract: Statement of problem
The purpose of this project is to implement an evidence based proposal project that incorporates team training of surgical team members including nursing, surgeons, physician assistants (PA), surgical technologists (ST), certified registered nurse anesthetists (CRNA), and anesthesiologists to improve the safety culture in the OR setting. The significance of this project affects three areas of nursing: 1.) clinical practice, 2.) education, and 3.) research.
The IOWA Model of Evidence-Based Practice was used.
Methodology
The study design used a descriptive, pilot design to measure teamwork perceptions of surgeons, PA’s, nurses, ST’s, anesthesiologists, and CRNA’s. The instrument used to measure the current teamwork perceptions is the Safety Attitudes Questionnaire (SAQ) (Sexton et al., 2003). The sample was a convenience sample of 139 participants. The survey was completed using survey Monkey.
Results
There exist significant differences in perceptions of teamwork ratings in the OR. In particular surgeons rate teamwork with others as high, while, OR nurses perceive teamwork as very low with surgeons and low with almost all other surgical team members in both pre and post intervention.
The significant difference seen in the post-intervention nursing scores could be the result of increased awareness of the problem, lack of communication and collaboration once the intervention was given. This critical finding indicates that further and more aggressive interventions need to be given to raise awareness in all surgical disciplines.
Conclusions
Nursing can begin by providing a supportive foundation to existing and new nurses with proper training and education on effective teamwork and its impact on patient outcomes. Next steps within the current organization is to introduce all existing staff and physicians to TeamSTEPPS training tools and how it can be used to have collaborative conversations about safety concerns and at the same time be heard.
Practice Implications
Nursing and medical schools need to begin introducing teamwork skills into there programs. A key concept of health care is prevention. Therefore academia has the responsibility to create a foundation for students, including teaching basic communication language that will enhance the teamwork relationships between future nurses and physicians. It is important to bring these groups together.
The Science of Cleaning Reusable Devices
Author:
Marcia Frieze, CEO, Case Medical
Abstract: When it comes to cleaning reusable surgical and medical devices, not all cleaners nor methods are created equal. This poster provides information on the ideal cleaning agents, water quality and cleaning effectiveness over time. This poster also addresses common myths vs. facts that allow users to make more informed decisions to increase efficiency and safety when deciding on a facility’s cleaning process.
Total Cost of Ownership - Definition and Reasons to Consider
Authors:
Rick McDaniel, Marketing , Marketing Manager , Getinge
Thomas Wetterberg , Marketing MBA, Marketing Manager , Getinge
Abstract: The poster and presentation will focus on the criteria to consider when analyzing the total cost of maintaining and running a pieced of capital equipment. The poster will list top criteria when reviewing such as: service plans, service cost on demand, technical training of internal clinical engineers, internal labor cost, OEM labor costs, travel time for OEM technician, parts costs and what are the parts that typically need to be replaced at yearly intervals, preventative maintenance cost and interval of PM (hours of use? Yearly?), clinical time used in a typical procedure, electric use, finance charges if using finance, percent of down time and the cost associated. The emphasis will be to include just the criteria with impact. Also focus will be on the equipment’s life cycle with the recommendation to buy durability. The poster will also look at the importance of utilizing certified technicians as well as OEM parts.
With regards to durability, the poster will review a hypothetical scenario involving a piece of capital equipment at the lowest price ($80,000) but with a lifespan of 6 years in comparison to a more durable piece of equipment ($100,000) with a lifespan of 10 years. Without estimating the cost of a possible increase in downtime, the cost of equipment goes from one unit at $10,000 per year (for ten years) to two units at $13,333 per year (for twelve years). This represents a 33% increase by going with the cheaper piece of equipment.
The presentation will also point out the importance of comparing the same criteria for each manufacturer. Left to their own, a manufacturer will define cost of ownership so as to favor their strengths. It is also important to review consumables to operate the equipment and if there are parts prone to damage when in use.
UroLift System Treatment
Author:
Lisa P. Jacob, MSN, RN, CNOR, Operating Room Nurse Manager, Michael E. DeBakey VA Medical Center
Abstract:
Urolift is a minimally invasive operative procedure for Benign Prostate Hyperplasia (BPH). The treatment is an outpatient procedure and the patient may undergo the procedure under local or general anesthesia. It provides another option for patients looking for an alternative to drug therapy or major surgery such as the Transurethral Resection of the Prostate (TURP). The treatment opens up the enlarged prostate out of the way by inserting small implants through the prostate.
Methods: The Urolift delivery device is placed through the urethra to access the enlarged prostate. Small implants are permanently placed to lift the enlarged prostate out if the way and increase the urethral opening. The implants are delivered through a needle that comes out of the Urolift delivery device and into the prostate. The Urolift delivery device is removed, leaving a more open urethra to provide symptom relief.
Results: Clinical data had shown that the Urolift system treatment is effective in relieving lower urinary tract symptoms due to enlarged prostate. Patients can experience improvement as early as two weeks. They report no erectile or ejaculatory dysfunction. Most symptoms are mild to moderate in severity and resolved within two to four weeks.
Conclusions: The goal of Urolift System treatment is to relieve urinary symptoms and resume normal daily activities.
Using Data to Improve Performance: What’s Your Analytics Strategy?
Authors:
Andi Dewes, BSN, RN, Chief Nursing Officer, Syus, Inc.
Jeff Belcher, BSN, RN, CSSM, Director of Surgical Services, Centennial Hills Hospital
Abstract:
Objectives:
• Discuss key performance measures and the impact of analytics
• Describe elements of a successful analytics strategy including tools and barriers, governance, communication and transparency
• Describe how one organization used analytics to understand and improve block utilization
Content summary:
Nurses have been involved with data collection and utilization for generations, and have been using a practical, repeatable process to provide evidence-based care to patients for decades. This same process can be followed when using analytics to identify, plan, and implement improvement initiatives. In the perioperative department, with increasing pressure to reduce cost, improve efficiency, and deliver exceptional patient care, all while keeping stakeholders satisfied, analytics and access to information are more important than ever. Perioperative leaders need tools to gather and analyze data, resources to help overcome barriers, communication plans for transparency and consistency, and a cohesive governance committee for strategic direction and support. Creating the right analytics strategy and following a practical analysis process, can be a powerful, easy to use way of transforming data into actionable information to achieve clinical and business goals. This poster will examine how one organization was able to improve block utilization and communication with surgeons through analytics.
Utilizing Technology to Decrease Discharge Time, Improve Patient Experience, and Promote Family Centered Care in a Same Day Surgery Unit
Authors:
Jennifer Simonetti , MSN, RN, CPN, Perioperative Nurse Educator, Magnet Program Director, Cohen Children's Medical Center
Ann Shea , BSN, RN, Nurse Manager, ASU, PST, MRI, Cohen Children's Medical Center
Tara Matz , MSN, RN, AE-C, Director Of Patient Care Services, ASU/PST/MRI, Neonatal and Pediatric Critical Care , Cohen Children's Medical Center
Aleece Rollison , BSN, RN, CPN , Pediatric Ambulatory Care Unit Clincal Nurse, Cohen Children's Medical Center
Michelle Pedalino , MSN, RN, CPN , Pediatric Ambulatory Care Unit Clincal Nurse, Cohen Children's Medical Center
Abstract: A family centered approach to the discharge process that utilizes a technology application which allows parents to stay united with their child, decreasing parental and child’s anxiety, discharge time and increasing satisfaction while their vehicle is brought to the front door. At this unit, over 400 patients are seen monthly. Due to safety regulations, pediatric patients require personal not public transportation home post-operatively. Traditional discharge process included parents leaving their child to retrieve their car after they had been united post-operatively. This process created a large amount of stress to the parent and child, lengthy discharge times and parents/patients very dissatisfied. Recognizing how this traumatic and timely discharge process can be, an inter-professional team worked to integrate a technology application that allows the parent and child to stay together once reunited. This new process includes the use of a computer application which is activated when the discharge order is communicated. A direct ticket is generated to valet services and the car is immediately placed in the cue for immediate pick up. While the car is retrieved the nurse is afforded golden time to review discharge instructions and answer questions. A educational plan was initiated for all staff and the integration of the new discharge process was seamless as it was user friendly and readily available. Initial pre-intervention data showed, time from discharge order to car of 34.45 minutes. After implementation post-intervention data reflected an 55% decrease in time to 14.5 minutes. Upon reevaluation of sustainment a 57.3% decrease was noted reflecting a new process time of 6.19 minutes for discharge order to car. With the implementation of this technology application into the discharge process the nurse is now able to maintain a family centered environment, which decreases their time off the unit, increases bed turnover and patient/family satisfaction.
Why is it Important to Evacuate Surgical Smoke
Author:
Robert W. Scroggins, BSN, RN, CMLSO, Clinical Programs Manager, Buffalo Filter
Abstract: The hazards of smoke have been known for decades. Research began in the 1950’s on tobacco smoke and culminated in 1964 with a report from the U.S. Surgeon General, Dr. Luther Terry. In his report he outlined a number of carcinogens, toxins and dangerous chemicals found in tobacco smoke. In the 1980’s research began in earnest on the contents of surgical smoke. It has been found that the components of surgical smoke are very similar, and in many cases, identical to tobacco smoke.
I have reviewed literature from 1980 to 2016 to find the most up to date information available on the hazardous content of surgical smoke and why it should be eliminated from the workplace of so many professionals just as tobacco smoke has been eliminated from places of employment and other public areas.
Surgical plume is a physical, biological and chemical hazard. There are ways to mitigate these hazards. Best practices include local exhaust ventilation (smoke evacuator), 0.1 micron N-95 respirators, universal precautions, strong policy, and education.
OR Manager Achievement Awards
Welcome to the OR Manager Achievement Awards Center
These prestigious awards are invaluable in recognizing the efforts of leaders in the perioperative industry; they foster a sense of community and continued motivation toward excellence.
Thank you for your nominations! The Planning Committee is reviewing the candidates and will be selecting the winners soon.

At the OR Manager Conference, we honor inspirational OR managers or directors every year with the OR Manager of the Year Award. Nominated by you, and hand selected by our Planning Committee and the OR Manager Advisory Board, the OR Manager of the Year is a champion of the perioperative suite.

Given to a rising star in OR management, the Emerging Leader Award will be presented in Orlando at the 2017 OR Manager Conference. This award was developed to recognize newer managers of the OR (five years or less experience) as they pave the way to the future of patient care and OR management.
Managers of the ASC face unique challenges on a daily basis. It’s because of this OR Manager felt as though it was time to call out the tremendous work that our colleagues who manage Ambulatory Surgery Centers be given their own accolade. Join us as we honor the top leaders in ambulatory services at the 2017 OR Manager Conference in Orlando!

Managing the OR takes more than just perioperative savvy, it also requires a strong business acumen; requiring complex logistical decisions, scheduling demands, analytical thinking, and a focus on the bottom-line. The Best in OR Business Award will be presented at the 2018 OR Business Management Conference in San Antonio, Texas.
The OR Manager of the Year recipient receives a complimentary registration to the OR Manager Conference, along with complimentary airfare and hotel.
Other award winners will receive a complimentary Value Package to the OR Manager Conference at the Gaylord Palms from October 2-4.
Congratulations to our 2016 OR Manager Awards recipients:

OR Manager of the Year
Patricia Ljubi, MBA, BA, RN
Director of Clinical and Perioperative Services
UG Geauga Medical Center

Emerging Leader Award
Megan Beaton, BSN, RN, CNOR
Director OR
UPMC Hamot

Ambulatory Services Achievement Award
Ellen Carpenter, BSN, RN
Nurse Manager Operating Room
Center for Advanced Medicine Ambulatory Surgery Center Long Island Jewish Medical Center/Northwell Health System
Best in OR Business Award
Vickie Stewart, MBA
Director, Business Operations, Peri-operative Services
University of Maryland Medical Center
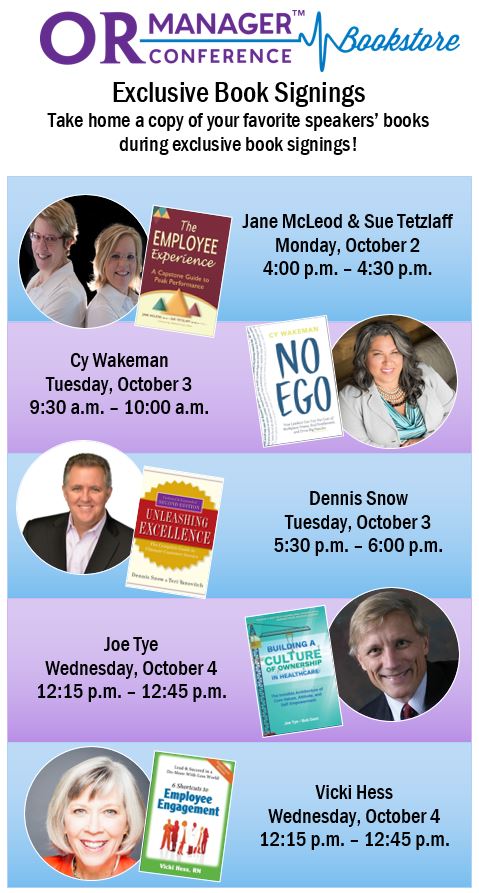

Attendee: Quick Info
Nominate a Leader for the OR Manager Awards
Quick Info
Location
Gaylord Palms Resort and Convention Center
Orlando, Florida
Date
October 2-4, 2017
CE Credits
Earn up to 19.0 CEs and 14.75 AEUs through workshops, breakout sessions, and keynotes. Additional credit hours can be earned through poster sessions and exhibitor presentations.
Tips for Award Submissions